The Truth About EHR API Integrations: Why the Future Isn’t Another Integration
Modern healthcare systems talk. At least, they’re supposed to.
On paper, EHR API integrations sound like the holy grail of healthcare tech: connect systems once, and data just flows. APIs (short for Application Programming Interfaces) let software exchange information automatically.
In theory, they give clinicians real-time access to labs, med lists, and notes. And for large health systems with robust IT teams, APIs deliver.
For small and midsized clinics, it’s a different story. EHR integrations are expensive, clunky, and complicated.
For many practices, the promise of real-time data and automated workflows still seems more like a dream than a reality.
The good news? There’s finally a way to skip the integrations altogether and still get seamless charting.
Why EHR API integrations matter
First, let’s dig into what’s working for EHR API integrations.
When systems can talk and share data, our medical history becomes something real and reliable.
- Real-time data exchange — Lab results, medication changes or imaging reports show up instantly.
- Workflow efficiency — API-based integrations reduce manual entry, eliminate duplicated efforts, and save clinicians from becoming admin.
- Unified patient view — Connecting disparate sources (EHRs, patient portals, apps) gives us a holistic picture of the patient.
- Regulatory alignment — With rising demand for interoperability and data access, APIs help organizations stay ahead of regulatory curves. For example, in 2020, the Office of the National Coordinator for Health Information Technology (ONC)’s interoperability rule began requiring certified EHRs to provide standardized APIs so patients and apps can access electronic health information.
The promise of interoperability sounds simple — but behind every connection lies a maze of technical frameworks that make those systems talk to each other. While powerful, these standards are implemented in ways that need robust IT and integration teams — which smaller clinics often don’t have.
EHR API integration standards
EHR API integration isn’t just about wiring two systems together — it’s about teaching them to speak the same language. To do that, healthcare relies on the set of standards that define how data moves between systems and what it means once it gets there.
Here are the core standards you’ll run into:
Tip: “Standards” aren’t just the data format. They include coding vocabularies , schemas, governance and version. According to Healthcare Information and Management Systems Society (HIMSS), there are multiple “levels” of interoperability — from foundational (just connecting systems) to semantic (shared meaning) and organizational/governance level.
These standards are the backbone of interoperability. They’re also a double-edged sword. Every layer of standardization, governance, and vendor oversight adds new cost and time commitments for the very clinics these systems are meant to help.
The hidden costs of “integration readiness”
Most clinics underestimate what it takes to become “integration ready.” And the costs go far beyond software licenses.
According to the Agency for Healthcare Research and Quality (AHRQ), health IT projects often require major up-front investment in staff training, workflow redesign, and ongoing data-quality maintenance. Even large, well-funded EHR programs face schedule delays, cost overruns, and and frustrated clinicians — so it’s no surprise that smaller practices struggle to justify similar investments. One AHRQ-funded study found that a five-physician clinic spent about $233,000. $230,000 from planning through the first year of EHR use.
- Implementation labor: Each API connection requires auditing source fields, mapping targets, and normalizing units
- Maintenance overhead: Every EHR update risks breaking connections and forcing new testing cycles.
- Staffing gaps: Many independent practices lack full-time IT personnel to oversee integrations.
- Opportunity cost: clinician and staff hours spent troubleshooting connections replace time for patients, documentation review, or follow-up.
And after all that work? The payoff still falls short.
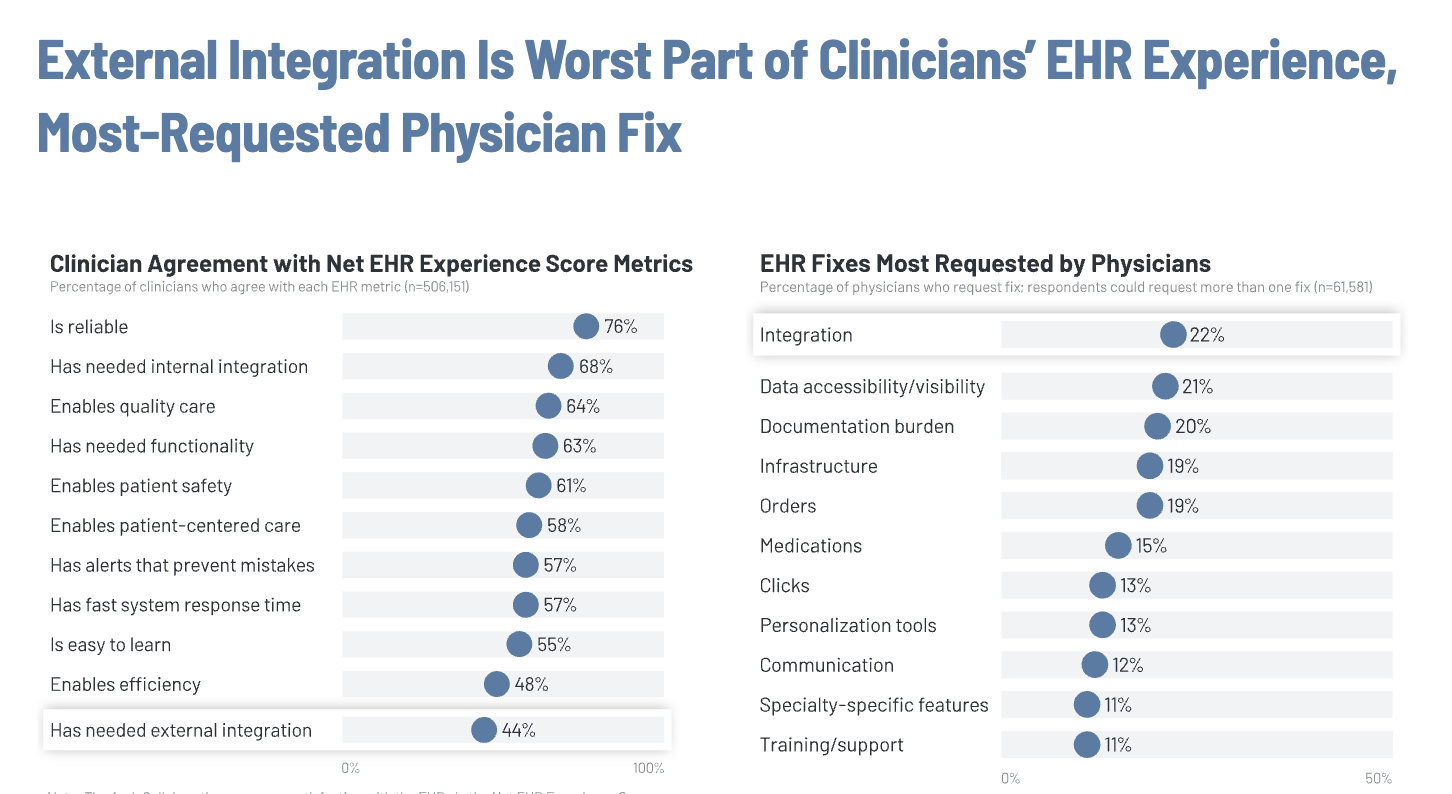
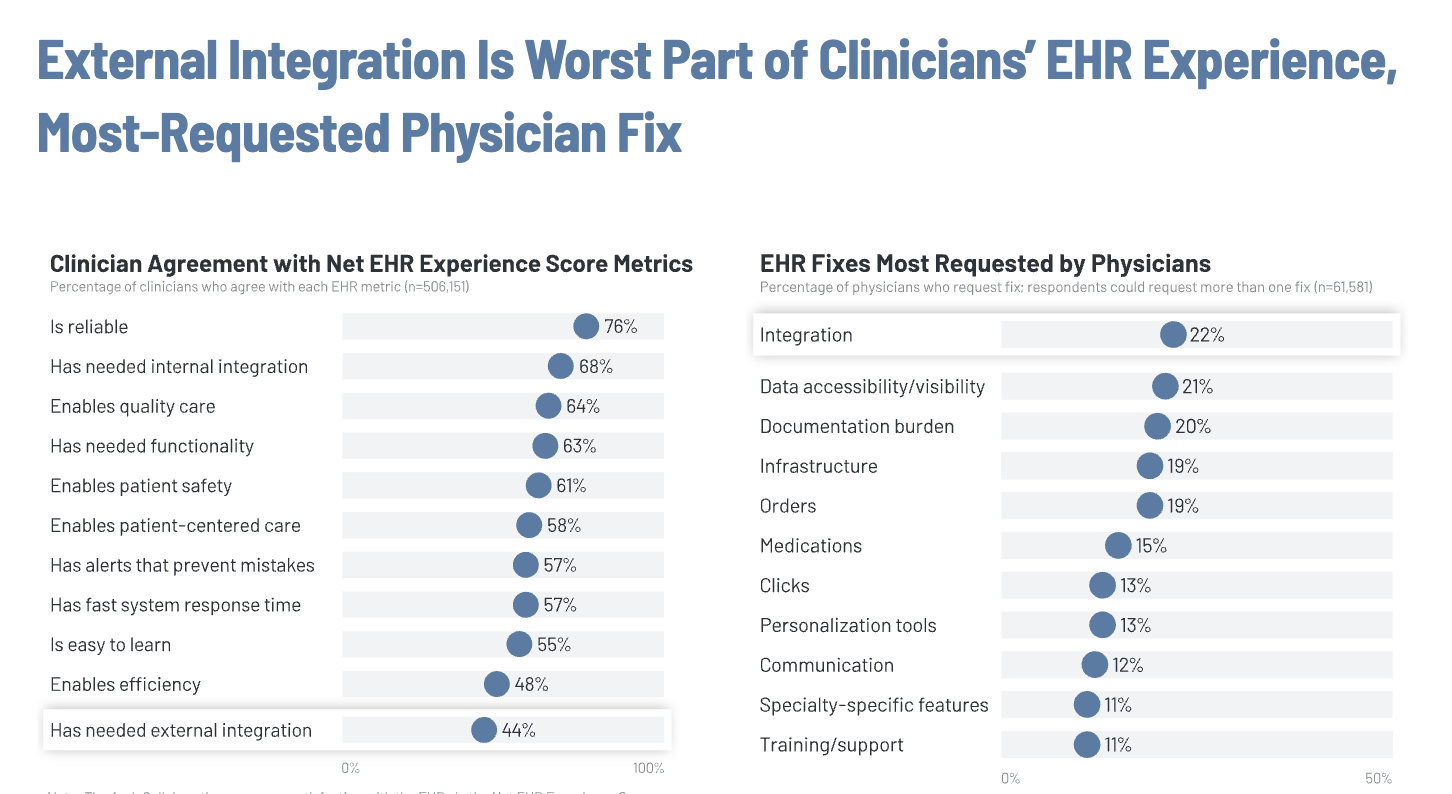
The 2024 KLAS Research EHR Interoperability Report found that only 44% of clinicians believe their EHR provides the expected level of integration with outside organizations, while 47% said they can’t quickly find important patient information from outside organizations.
That’s why clinicians are looking for alternatives that don’t rely on APIs at all — ones that make interoperability feel invisible, not impossible.
A new model: agentic AI and “anti-integrations”
Freed built EHR push to flip the traditional integration model on its head.
This new feature is part of Freed’s Chrome extension, and sits on top of any browser-based EHR.
Instead of waiting for every EHR to expose the exact API needed, Freed’s EHR AI agent navigates the EHR directly — placing the finalized note where it belongs.
That’s because agentic AI doesn’t just move data between systems, agentic AI understands context, takes action, and learns from its environment.
“Integrations disproportionately serve large systems with budgets and IT teams. Small practices shouldn’t have to wait a year for interoperability. They deserve usable solutions today.” — Erez Druk, Freed CEO
Freed’s “anti-integration” model doesn’t replace APIs — it bypasses their bottlenecks. The underlying agentic AI technology has matured to the point that it’s reliable, fast, and continually improving based on clinician feedback and evaluation.
How EHR push’s agentic AI works in practice
Once a clinician finalizes a note in Freed’s AI scribe, they open the extension and click Push to EHR.
The agent maps structured sections of the note to the correct fields in the chart and inserts them. We have multiple checkpoints in that process to ensure accurate mapping and transfer.
If anything looks off, it fails safely and does not attempt to transfer. And the team is constantly measuring the quality and latency of pushes, as well as reviewing user feedback to understand areas to improve.
Why an agentic AI platform matters
This means freedom from the IT friction that’s held back small and mid-sized practices.
- Low setup time: Works day one with any browser-based EHR
- No IT dependency: No vendor coordination or maintenance
- Immediate ROI: Practices can see the difference immediately
It’s a technology shift that levels the playing field, giving small practices the same efficiency once reserved for large hospital systems.
EHRs win too: they get reduced integration costs, faster time-to-market, and easier connectivity with top-tier scribe solutions.
An evolution from API integrations
APIs will always have their place in healthcare. But they shouldn’t be the only path to interoperability.
EHR push is in beta through the remainder of 2025. But the path is clear:
- First, GA (general availability)
- Clinician adoption and retention
- Scale from thousands to tens of thousands of daily agent sessions
Note: GA means the product is officially out of beta and ready for everyday use. It’s like when a hospital rolls out a new EHR system after testing — stable and reliable.
In the long run, we want to extend these agentic capabilities to build a world where clinicians spend their time on care — while background agents handle the charting, orders, prescriptions, and follow-ups.
EHR push shows what’s possible when we think beyond the old EHR API systems, and start building for clinicians.
Ready to see what anti-integration looks like? Check out EHR push.
Table of Contents
Modern healthcare systems talk. At least, they’re supposed to.
On paper, EHR API integrations sound like the holy grail of healthcare tech: connect systems once, and data just flows. APIs (short for Application Programming Interfaces) let software exchange information automatically.
In theory, they give clinicians real-time access to labs, med lists, and notes. And for large health systems with robust IT teams, APIs deliver.
For small and midsized clinics, it’s a different story. EHR integrations are expensive, clunky, and complicated.
For many practices, the promise of real-time data and automated workflows still seems more like a dream than a reality.
The good news? There’s finally a way to skip the integrations altogether and still get seamless charting.
Why EHR API integrations matter
First, let’s dig into what’s working for EHR API integrations.
When systems can talk and share data, our medical history becomes something real and reliable.
- Real-time data exchange — Lab results, medication changes or imaging reports show up instantly.
- Workflow efficiency — API-based integrations reduce manual entry, eliminate duplicated efforts, and save clinicians from becoming admin.
- Unified patient view — Connecting disparate sources (EHRs, patient portals, apps) gives us a holistic picture of the patient.
- Regulatory alignment — With rising demand for interoperability and data access, APIs help organizations stay ahead of regulatory curves. For example, in 2020, the Office of the National Coordinator for Health Information Technology (ONC)’s interoperability rule began requiring certified EHRs to provide standardized APIs so patients and apps can access electronic health information.
The promise of interoperability sounds simple — but behind every connection lies a maze of technical frameworks that make those systems talk to each other. While powerful, these standards are implemented in ways that need robust IT and integration teams — which smaller clinics often don’t have.
EHR API integration standards
EHR API integration isn’t just about wiring two systems together — it’s about teaching them to speak the same language. To do that, healthcare relies on the set of standards that define how data moves between systems and what it means once it gets there.
Here are the core standards you’ll run into:
Tip: “Standards” aren’t just the data format. They include coding vocabularies , schemas, governance and version. According to Healthcare Information and Management Systems Society (HIMSS), there are multiple “levels” of interoperability — from foundational (just connecting systems) to semantic (shared meaning) and organizational/governance level.
These standards are the backbone of interoperability. They’re also a double-edged sword. Every layer of standardization, governance, and vendor oversight adds new cost and time commitments for the very clinics these systems are meant to help.
The hidden costs of “integration readiness”
Most clinics underestimate what it takes to become “integration ready.” And the costs go far beyond software licenses.
According to the Agency for Healthcare Research and Quality (AHRQ), health IT projects often require major up-front investment in staff training, workflow redesign, and ongoing data-quality maintenance. Even large, well-funded EHR programs face schedule delays, cost overruns, and and frustrated clinicians — so it’s no surprise that smaller practices struggle to justify similar investments. One AHRQ-funded study found that a five-physician clinic spent about $233,000. $230,000 from planning through the first year of EHR use.
- Implementation labor: Each API connection requires auditing source fields, mapping targets, and normalizing units
- Maintenance overhead: Every EHR update risks breaking connections and forcing new testing cycles.
- Staffing gaps: Many independent practices lack full-time IT personnel to oversee integrations.
- Opportunity cost: clinician and staff hours spent troubleshooting connections replace time for patients, documentation review, or follow-up.
And after all that work? The payoff still falls short.
The 2024 KLAS Research EHR Interoperability Report found that only 44% of clinicians believe their EHR provides the expected level of integration with outside organizations, while 47% said they can’t quickly find important patient information from outside organizations.
That’s why clinicians are looking for alternatives that don’t rely on APIs at all — ones that make interoperability feel invisible, not impossible.
A new model: agentic AI and “anti-integrations”
Freed built EHR push to flip the traditional integration model on its head.
This new feature is part of Freed’s Chrome extension, and sits on top of any browser-based EHR.
Instead of waiting for every EHR to expose the exact API needed, Freed’s EHR AI agent navigates the EHR directly — placing the finalized note where it belongs.
That’s because agentic AI doesn’t just move data between systems, agentic AI understands context, takes action, and learns from its environment.
“Integrations disproportionately serve large systems with budgets and IT teams. Small practices shouldn’t have to wait a year for interoperability. They deserve usable solutions today.” — Erez Druk, Freed CEO
Freed’s “anti-integration” model doesn’t replace APIs — it bypasses their bottlenecks. The underlying agentic AI technology has matured to the point that it’s reliable, fast, and continually improving based on clinician feedback and evaluation.
How EHR push’s agentic AI works in practice
Once a clinician finalizes a note in Freed’s AI scribe, they open the extension and click Push to EHR.
The agent maps structured sections of the note to the correct fields in the chart and inserts them. We have multiple checkpoints in that process to ensure accurate mapping and transfer.
If anything looks off, it fails safely and does not attempt to transfer. And the team is constantly measuring the quality and latency of pushes, as well as reviewing user feedback to understand areas to improve.
Why an agentic AI platform matters
This means freedom from the IT friction that’s held back small and mid-sized practices.
- Low setup time: Works day one with any browser-based EHR
- No IT dependency: No vendor coordination or maintenance
- Immediate ROI: Practices can see the difference immediately
It’s a technology shift that levels the playing field, giving small practices the same efficiency once reserved for large hospital systems.
EHRs win too: they get reduced integration costs, faster time-to-market, and easier connectivity with top-tier scribe solutions.
An evolution from API integrations
APIs will always have their place in healthcare. But they shouldn’t be the only path to interoperability.
EHR push is in beta through the remainder of 2025. But the path is clear:
- First, GA (general availability)
- Clinician adoption and retention
- Scale from thousands to tens of thousands of daily agent sessions
Note: GA means the product is officially out of beta and ready for everyday use. It’s like when a hospital rolls out a new EHR system after testing — stable and reliable.
In the long run, we want to extend these agentic capabilities to build a world where clinicians spend their time on care — while background agents handle the charting, orders, prescriptions, and follow-ups.
EHR push shows what’s possible when we think beyond the old EHR API systems, and start building for clinicians.
Ready to see what anti-integration looks like? Check out EHR push.
FAQs
Frequently asked questions from clinicians and medical practitioners.
Does Freed integrate with EHRs and EMRs?
Do I need IT support to set up EHR push?
Does EHR push work with my specific EHR?
Is EHR push free?
Can I customize how my notes appear in my EHR?
Related content






