What is the Benefit of Using SOAP notes?
SOAP notes are a hot topic on the Med School subreddit. To some, they're rigid and outdated. To others, they're the holy grail.
SOAP was the first format for a reason, but we're in a new era. Are they still worth using? Let’s break down their benefits, how they compare to other formats, and ways to make them work better for modern clinicians.
What are SOAP Notes?
If you're in patient care, you're no stranger to SOAP notes. Love them or loathe them, they’ve been the standard for medical documentation for decades.
SOAP stands for:
- Subjective: The patient’s history, symptoms, and reported concerns.
- Objective: Measurable data, including:
- Vital signs
- Lab results
- Physical exam findings
- Assessment and Plan : The clinician’s analysis of the patient’s condition and next steps for treatment or management.
The history of SOAP notes
SOAP notes were introduced in the 1960s by Dr. Larry Weed, who saw the need for a more structured approach to medical documentation. Before SOAP, clinicians used unstructured, often illegible notes that made communication and record-keeping chaotic.
“The human mind simply cannot carry all of the information about all of the patients in the practice” — Dr. Larry Weed
By creating a standardized format, SOAP notes brought order to the medical record for the first time.
Weed's SOAP methodology was one branch of the Problem-Oriented Medical Record (POMR) system —a standardized way to store and update medical history.
SOAP note benefits: Why clinicians still use them
SOAP notes might get a bad rap, but they're popular for a reason. Here's why:
1. Standardization
In a fast-paced clinical setting, structure is a lifesaver. SOAP notes ensure that key details are documented consistently, making it easier for providers to track a patient’s progress over time.
They also streamline communication between healthcare providers, so that all necessary information is available for clinical decision-making and billing — without unnecessary clutter.
2. Easily shareable
SOAP notes aren’t just for the clinician who writes them. They keep all healthcare professionals on the same page, reducing miscommunication and ensuring continuity of care.
The electronic health record (EHR) needs us to document patient information in a specific way, and that's usually already framed in SOAP format.
3. Legal protection and compliance
Accurate documentation isn’t just good practice — it’s a safeguard. SOAP notes serve as legal records of diagnoses, treatments, and clinical reasoning, protecting both clinicians and patients in case of disputes or insurance claims.
This document is crucial as it may benefit both the clinician and the patient, in the event of a malpractice lawsuit or denial of insurance coverage.
4. A clear summary for patient care
SOAP notes don’t just help healthcare providers—they help patients, too. A well-structured note provides a clear, concise medical summary, allowing patients to better understand their health and treatment plan.
By keeping information organized, SOAP notes can also flag potential concerns early, ensuring necessary follow-ups aren’t missed.
How SOAP notes can evolve
SOAP notes have been around for decades, and while the core idea still holds up, documentation needs have changed.
So, what’s next?
1. APSO notes: flipping the format
Remember our friends on Reddit earlier? Some had a strong preference for APSO notes, which reorders the format to Assessment, Plan, Subjective, and Objective.
Why the shift? Many providers find that leading with the assessment and plan makes the note more readable and actionable.
In fact, an APSO adoption study across the healthcare system found that 80% of clinicians were “satisfied” or “very satisfied” with the new format.
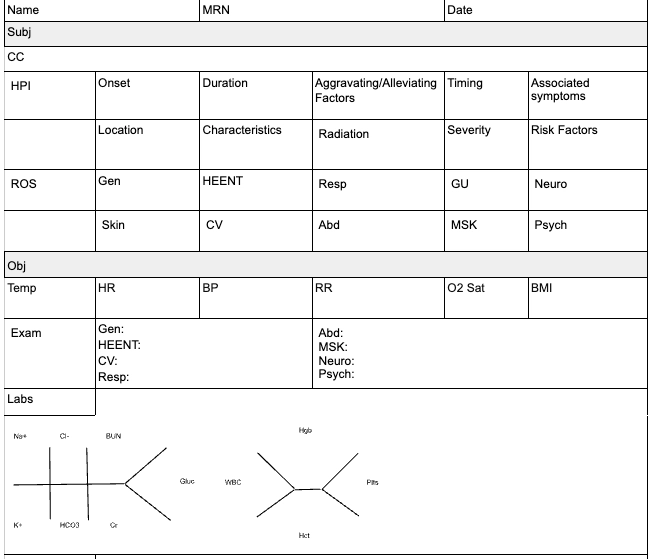
2. SOAP note templates: Structure without the struggle.
One simple way to make SOAP notes easier? Use a template.
A well-designed SOAP note template ensures consistency while cutting down on unnecessary typing.
Here's a free template you can download and use today!
2. Medical dictation software: Hands-free efficiency
Typing notes takes time — time that could be spent with patients (or having dinner at home).
That’s why medical dictation software is gaining traction. The global market for medical speech recognition is forecasted to reach USD 5.58 billion by 2035.
3. AI scribes
If medical dictation software is the present, then AI scribes are the future. These artificial intelligence programs use natural language processing to transcribe and organize medical notes in real time.
AI scribes can also assist with tasks like identifying potential drug interactions or suggesting appropriate codes for billing purposes.
While still in its early stages, AI scribes have shown great potential in improving documentation efficiency and reducing administrative burdens for healthcare professionals.
In another study, AI scribes were found to encourage more patient-focused encounters, as healthcare providers were not distracted by the task of taking notes.
Wrapping Up
SOAP notes aren’t going anywhere, but they are evolving. As technology advances, healthcare professionals have more options to streamline documentation and do what they love — on and off the clock.
Ready to spend less time on notes and more time with patients? Try out the Freed free trial today. No credit card required.
Table of Contents
SOAP notes are a hot topic on the Med School subreddit. To some, they're rigid and outdated. To others, they're the holy grail.
SOAP was the first format for a reason, but we're in a new era. Are they still worth using? Let’s break down their benefits, how they compare to other formats, and ways to make them work better for modern clinicians.
What are SOAP Notes?
If you're in patient care, you're no stranger to SOAP notes. Love them or loathe them, they’ve been the standard for medical documentation for decades.
SOAP stands for:
- Subjective: The patient’s history, symptoms, and reported concerns.
- Objective: Measurable data, including:
- Vital signs
- Lab results
- Physical exam findings
- Assessment and Plan : The clinician’s analysis of the patient’s condition and next steps for treatment or management.
The history of SOAP notes
SOAP notes were introduced in the 1960s by Dr. Larry Weed, who saw the need for a more structured approach to medical documentation. Before SOAP, clinicians used unstructured, often illegible notes that made communication and record-keeping chaotic.
“The human mind simply cannot carry all of the information about all of the patients in the practice” — Dr. Larry Weed
By creating a standardized format, SOAP notes brought order to the medical record for the first time.
Weed's SOAP methodology was one branch of the Problem-Oriented Medical Record (POMR) system —a standardized way to store and update medical history.
SOAP note benefits: Why clinicians still use them
SOAP notes might get a bad rap, but they're popular for a reason. Here's why:
1. Standardization
In a fast-paced clinical setting, structure is a lifesaver. SOAP notes ensure that key details are documented consistently, making it easier for providers to track a patient’s progress over time.
They also streamline communication between healthcare providers, so that all necessary information is available for clinical decision-making and billing — without unnecessary clutter.
2. Easily shareable
SOAP notes aren’t just for the clinician who writes them. They keep all healthcare professionals on the same page, reducing miscommunication and ensuring continuity of care.
The electronic health record (EHR) needs us to document patient information in a specific way, and that's usually already framed in SOAP format.
3. Legal protection and compliance
Accurate documentation isn’t just good practice — it’s a safeguard. SOAP notes serve as legal records of diagnoses, treatments, and clinical reasoning, protecting both clinicians and patients in case of disputes or insurance claims.
This document is crucial as it may benefit both the clinician and the patient, in the event of a malpractice lawsuit or denial of insurance coverage.
4. A clear summary for patient care
SOAP notes don’t just help healthcare providers—they help patients, too. A well-structured note provides a clear, concise medical summary, allowing patients to better understand their health and treatment plan.
By keeping information organized, SOAP notes can also flag potential concerns early, ensuring necessary follow-ups aren’t missed.
How SOAP notes can evolve
SOAP notes have been around for decades, and while the core idea still holds up, documentation needs have changed.
So, what’s next?
1. APSO notes: flipping the format
Remember our friends on Reddit earlier? Some had a strong preference for APSO notes, which reorders the format to Assessment, Plan, Subjective, and Objective.
Why the shift? Many providers find that leading with the assessment and plan makes the note more readable and actionable.
In fact, an APSO adoption study across the healthcare system found that 80% of clinicians were “satisfied” or “very satisfied” with the new format.
2. SOAP note templates: Structure without the struggle.
One simple way to make SOAP notes easier? Use a template.
A well-designed SOAP note template ensures consistency while cutting down on unnecessary typing.
Here's a free template you can download and use today!
2. Medical dictation software: Hands-free efficiency
Typing notes takes time — time that could be spent with patients (or having dinner at home).
That’s why medical dictation software is gaining traction. The global market for medical speech recognition is forecasted to reach USD 5.58 billion by 2035.
3. AI scribes
If medical dictation software is the present, then AI scribes are the future. These artificial intelligence programs use natural language processing to transcribe and organize medical notes in real time.
AI scribes can also assist with tasks like identifying potential drug interactions or suggesting appropriate codes for billing purposes.
While still in its early stages, AI scribes have shown great potential in improving documentation efficiency and reducing administrative burdens for healthcare professionals.
In another study, AI scribes were found to encourage more patient-focused encounters, as healthcare providers were not distracted by the task of taking notes.
Wrapping Up
SOAP notes aren’t going anywhere, but they are evolving. As technology advances, healthcare professionals have more options to streamline documentation and do what they love — on and off the clock.
Ready to spend less time on notes and more time with patients? Try out the Freed free trial today. No credit card required.
FAQs
Frequently asked questions from clinicians and medical practitioners.
What are the advantages of using the SOAP module of documentation?
What is the purpose of the SOAP method?
What is the Objective for SOAP notes?
Why is a clear SOAP note important to the medical coder?
Related content