9 Best AI Scribes for Psychiatrists [2026] Reviews, Compliance, Features
No matter the visit or client, charting eats our time. Between medication management, progress notes, and therapy portions of visits, it’s easy to lose another hour to documentation after-clinic.
AI scribes have matured quickly since 2024. A 2025 JAMA Network Open study found ambient documentation tools reduced clinician after-hours charting by 41% and improved professional fulfillment scores by 53%—with even greater gains in high-documentation specialties like psych.
Today’s psychiatry‑friendly platforms can:
- Listen to your in-person or telehealth sessions
- Summarize the essential clinical points
- Draft a note that respects both HIPAA and your personal documentation style.
Below is a psychiatry‑focused comparison of leading AI scribe tools as of 2026, based on firsthand clinician reviews on Reddit, G2, and other internet platforms.
Best AI scribes for psychiatrists, at a glance
How we evaluated AI scribes for psychiatrists
This roundup was built around how AI scribes perform in real psychiatric practice, not how they look in a sales deck. For each tool, the evaluation centered on:
- What psychiatrists, residents, and PMHNPs report about day‑to‑day use in clinic, including where tools actually save time and where they get in the way. These findings align with Mass General Brigham's 2025 analysis showing 78% of clinicians using ambient scribes reported less cognitive burden during visits.
- How well notes capture psychiatry‑specific elements: MSE, risk and safety language, psychotherapy themes, and medication rationale—not just a generic HPI.
- The editing load before a note is safe to sign and bill, especially for complex follow‑ups and crisis visits.
Platform fit also mattered:
- Whether the scribe works for common psychiatry setups (solo outpatient, group practices, community mental health, and hospital‑based services).
- How tightly it is tied to a single EHR versus flexible enough to follow psychiatrists across roles or organizations.
- Its stance on privacy and consent in mental health settings, including how recordings and transcripts are handled over time.
The aim was not to name one “best” product, but to map the trade‑offs psychiatrists actually face when choosing AI scribes that reduce documentation burden while still supporting sound clinical judgment.
What is an AI scribe for psychiatrists?
AI scribes for psychiatry turn visits into draft clinical notes — covering HPI, MSE, risk assessment, and treatment plan—using conversation, dictation, or structured input. They cut after-hours charting while keeping notes clinically sound and billable.
Psychiatry tools fall into four main types:
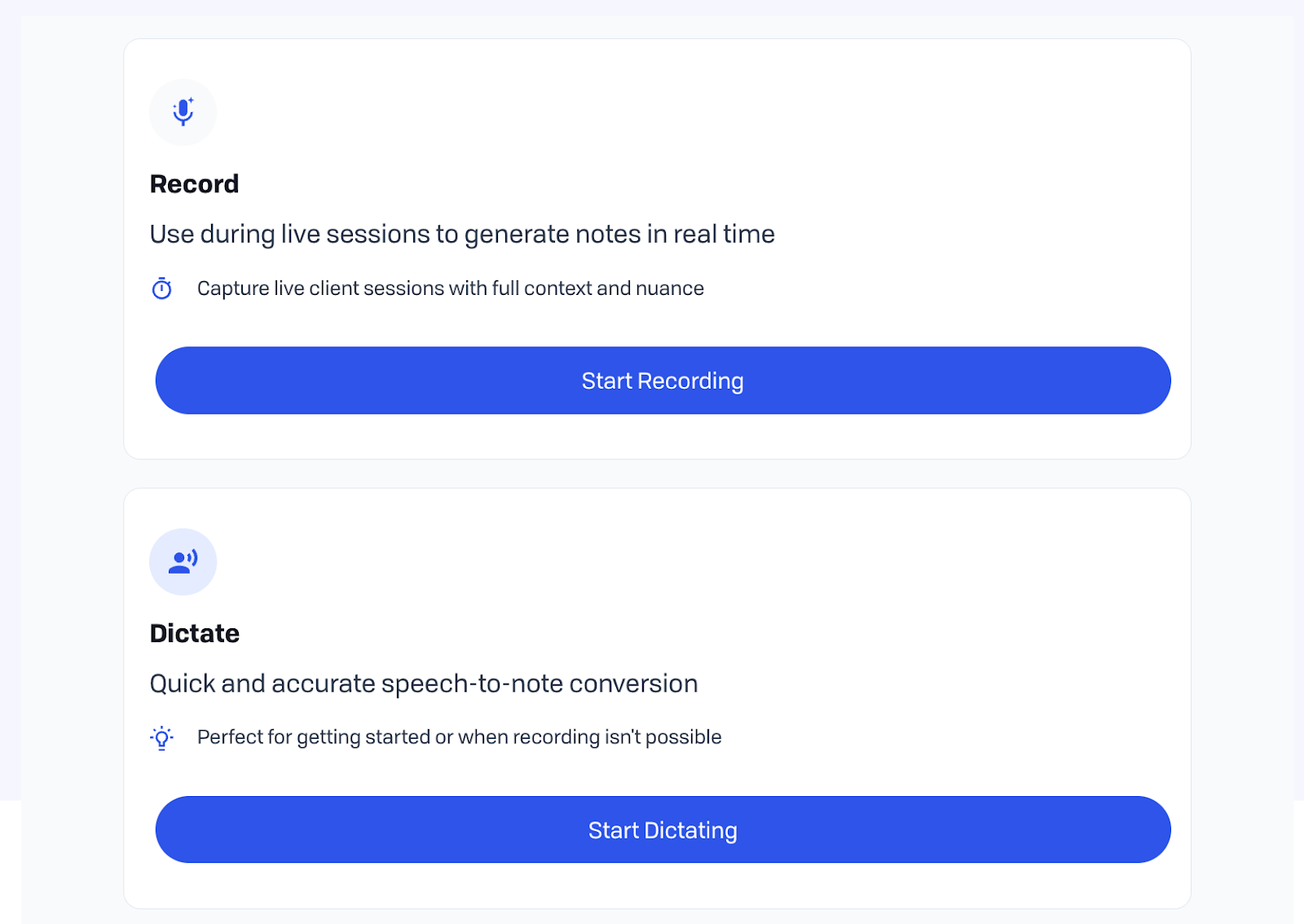
Ambient AI scribes
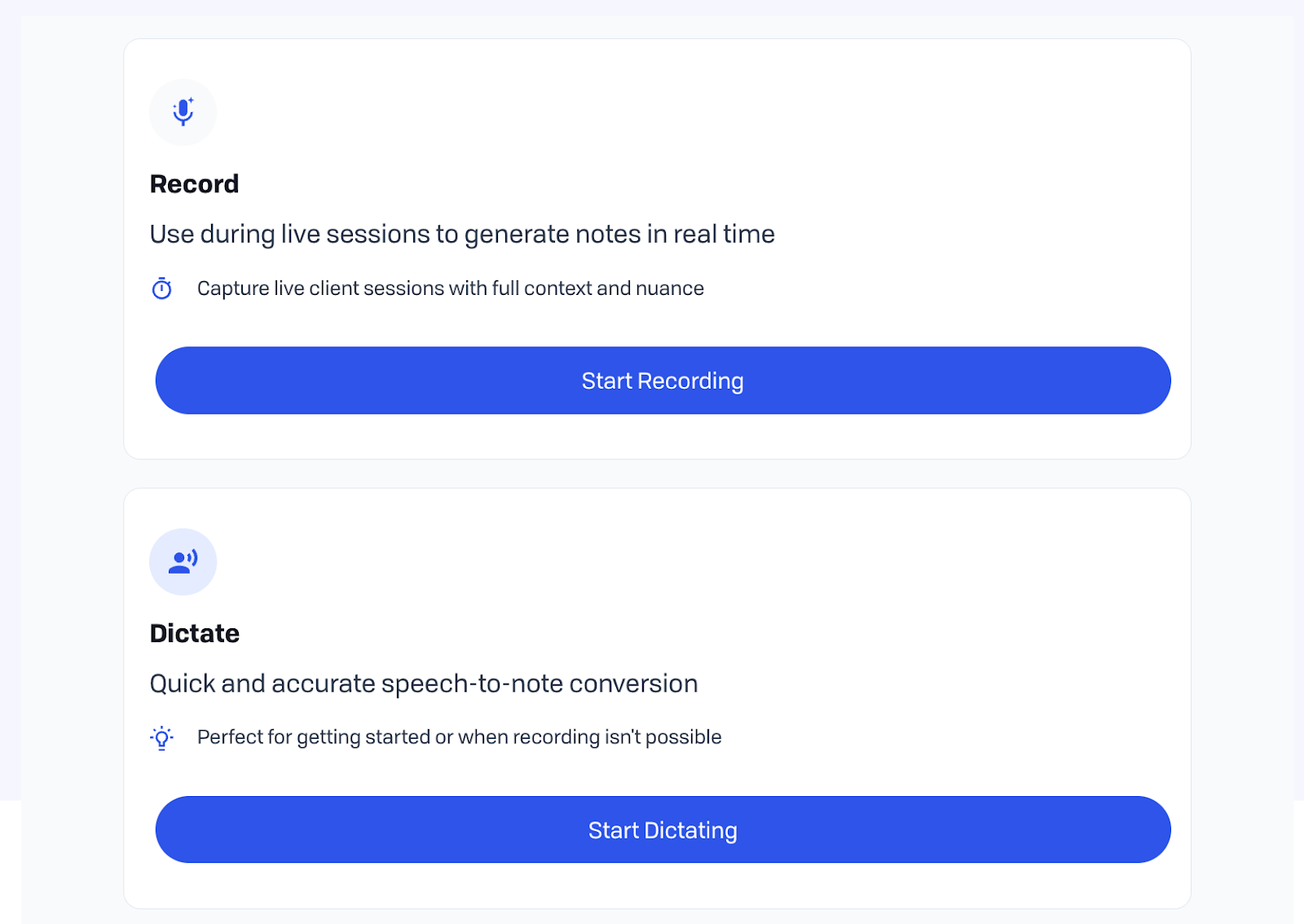
Listen live (in-person/telepsychiatry) to generate drafts from dialogue, reducing memory reconstruction of MSE or risk language. Freed and Abridge are examples.
Dictation-based tools
Post-visit verbal summary becomes structured SOAP/DAP notes. TherapyNotes AI and similar tools require recall but beat typing.
Prompt-based tools
Type key points (symptoms, meds, plan) for instant note drafts. Best for organized med-checks, less helpful during complex visits.
Measurement-driven tools
Use PHQ-9/GAD-7 scores plus text for progress notes tied to outcomes. Blueprint fits insurance-heavy psychiatry but limits narrative.
AI scribe options for psychiatrists
1. Freed
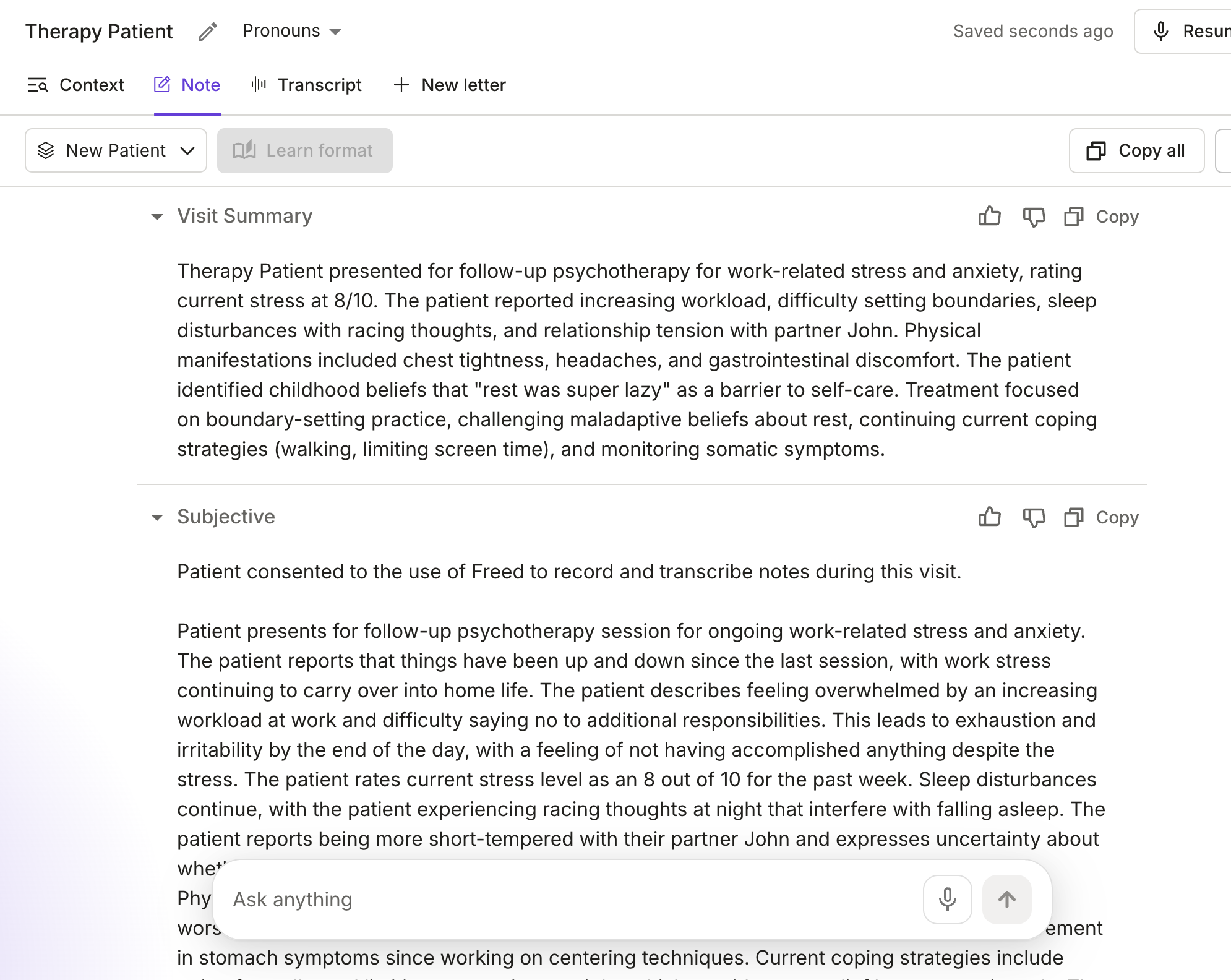
Freed is an ambient AI medical scribe designed to handle the realities of psychiatric visits — long conversations, nuanced mental status exams, medication management, and sensitive risk language — without forcing you to change how you practice or which EHR you use. The tool is HIPAA and HITECH compliant with industry-leading security standards.
Clinicians on Reddit describe Freed as follows: “the note this thing generated was precise, comprehensive, well-written and actually sounded like me. I was blown away. It would have taken me an easy 30 minutes to write a similar note.”
Freed listens to in‑person or telepsychiatry encounters and turns the conversation into clean narrative or SOAP‑style, customizable notes you can drop into virtually any web‑based EHR.
Freed’s EHR push feature allows a one-click push to any web-based EHR through its Chrome Extension, including Simple Practice, PracticeFusion, Athena Health and more.
One psychiatric clinician writes, “I was getting burned out, but that all changed with Freed. Now visits feel like I have a personal scribe in the background capturing every detail, freeing me to be 100% present with my patients. It’s far more efficient to review and edit a note already structured in SOAP format than write one from memory. I’ve been freed!”
Best for
- Psychiatrists and PMHNPs who want strong HPI, MSE, and plan drafts from live visits without switching EHRs
- Clinicians who prefer flat, predictable monthly pricing over per‑minute audio charges
Not as great for
- Larger hospital organizations
Pros
- Customizable templates that learn from your edits
- Advanced features like smart visit prep and patient letters, referrals, and more
- HIPAA‑compliant with BAAs on paid plans
- Paragraph‑style notes that often need only light editing, according to multiple Reddit and G2 reviewers
- Works across devices and fits with workflows like Zoom, so you can use it for both in‑person and telehealth sessions
Cons
- Free trial lasts only 7 days, no permanent free tier
2. TherapyNotes AI
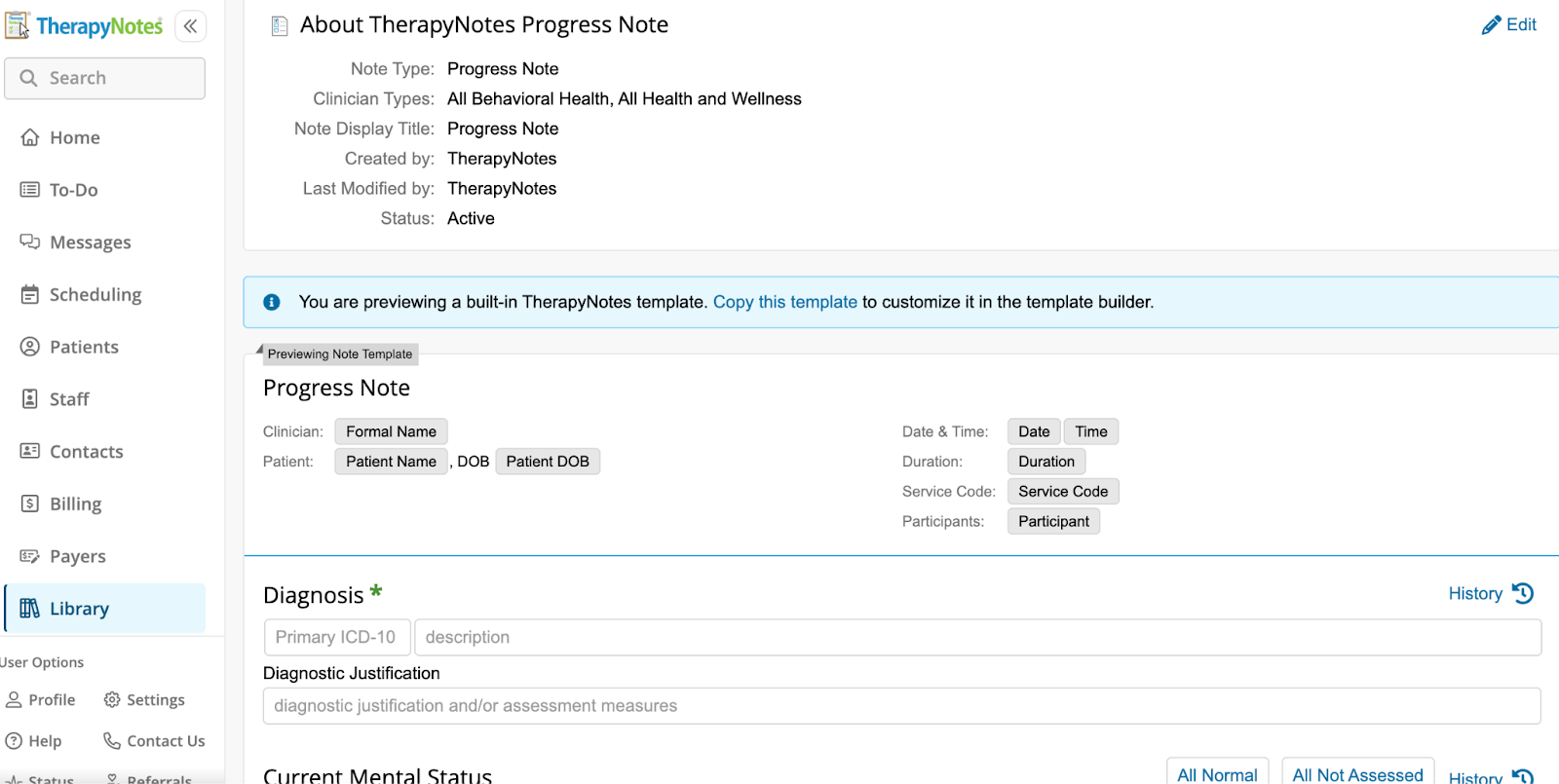
Many psychiatrists rely on TherapyNotes for scheduling, billing, and documentation. Its AI TherapyFuel functionality gives those users a built-in way to generate note drafts through AI, within the same EHR. It takes dictation or typed summaries and produces SOAP or DAP‑style notes directly.
One reddit user notes, “It definitely has some flaws, but it has made documentation much easier. It has helped me to stay more on top of note taking. I always read through and edit as necessary, but it does well.”
Best for
- Psychiatric practitioners who already use TherapyNotes and want AI support without adding another standalone tool
- Practices that prefer to keep billing, documentation, and AI‑generated drafts inside a single HIPAA‑compliant platform
Not as great for
- Clinicians using other EHRs or non‑EHR workflows, since the AI is not available as a separate product
- Psychiatrists who want highly nuanced, specialty‑tuned language for complex MSEs or psychodynamic notes rather than more generic drafts
Pros
- Embedded directly in TherapyNotes, avoiding copy‑and‑paste and keeping everything in one system
- Supports common mental‑health formats like SOAP and DAP for both therapy and med‑management visits
- Includes AI settings and consent language in the same place you manage the rest of your notes
Cons
- Independent reviews characterize it as “good but generic,” meaning you still need to refine tone and nuance
- Available only inside TherapyNotes, so you cannot use it if your practice runs on other platforms
3. Blueprint
Blueprint is not a traditional ambient scribe, but it uses standardized outcome measures (like PHQ‑9, GAD‑7, and related scales) plus brief text to generate structured progress notes and track symptom change over time in psychiatric care. That makes it especially appealing in insurance‑heavy, measurement‑based psychiatry, where tying documentation to validated instruments is a constant ask.
One Reddit user notes, “I use Blueprint and I love it. It’s HIPAA compliant, doesn’t sell the info, is a private company….It simply organizes my thoughts in a way that’s more coherent. You can add or delete as you wish and you should definitely read everything it generates from your notes to be sure it’s correct.”
Best for
- Psychiatrists and PMHNPs in clinics where payers expect regular use of validated scales and formal measurement‑based care
- Practices that want dashboards showing symptom trajectories, engagement, and outcomes alongside their notes
Not as great for
- Private‑pay or boutique practices where measurement scales are used infrequently
- Psychiatrists who prefer free‑form, psychodynamic‑style notes and rich process descriptions rather than scale‑anchored language
Pros
- Builds notes from rating‑scale data plus text, clearly linking documentation to treatment goals, severity, and outcomes for audits and payers
- Offers progress charts and other measurement‑based care tools that help visualize change over time
- Integrates with some EHRs, reducing manual efforts
Cons
- Note language can feel constrained by the underlying scales and may not capture nuanced psychodynamics or complex interpersonal themes
- Per‑client or per‑use pricing can add up for psychiatrists managing large, high‑acuity caseloads
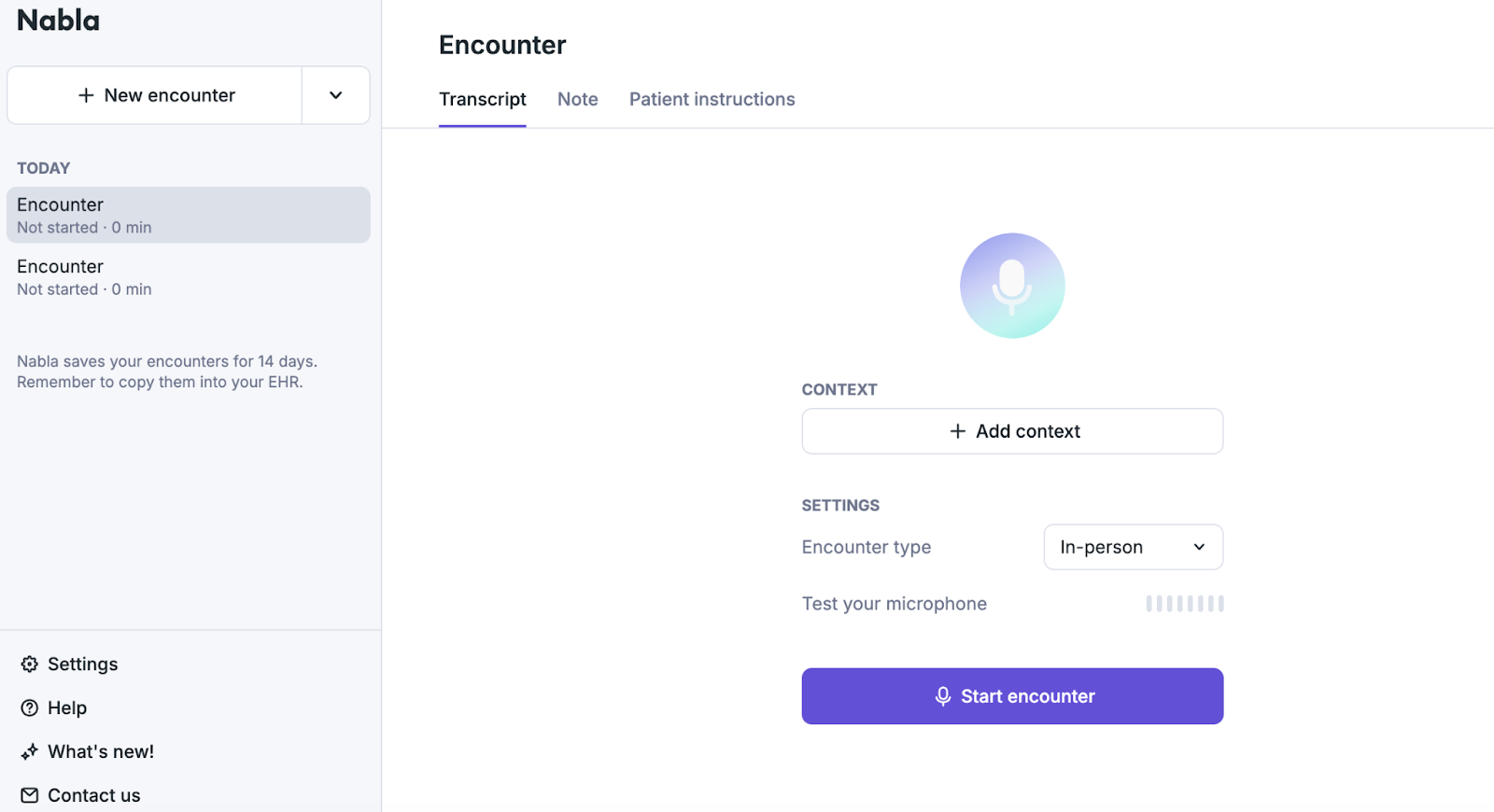
4. Nabla
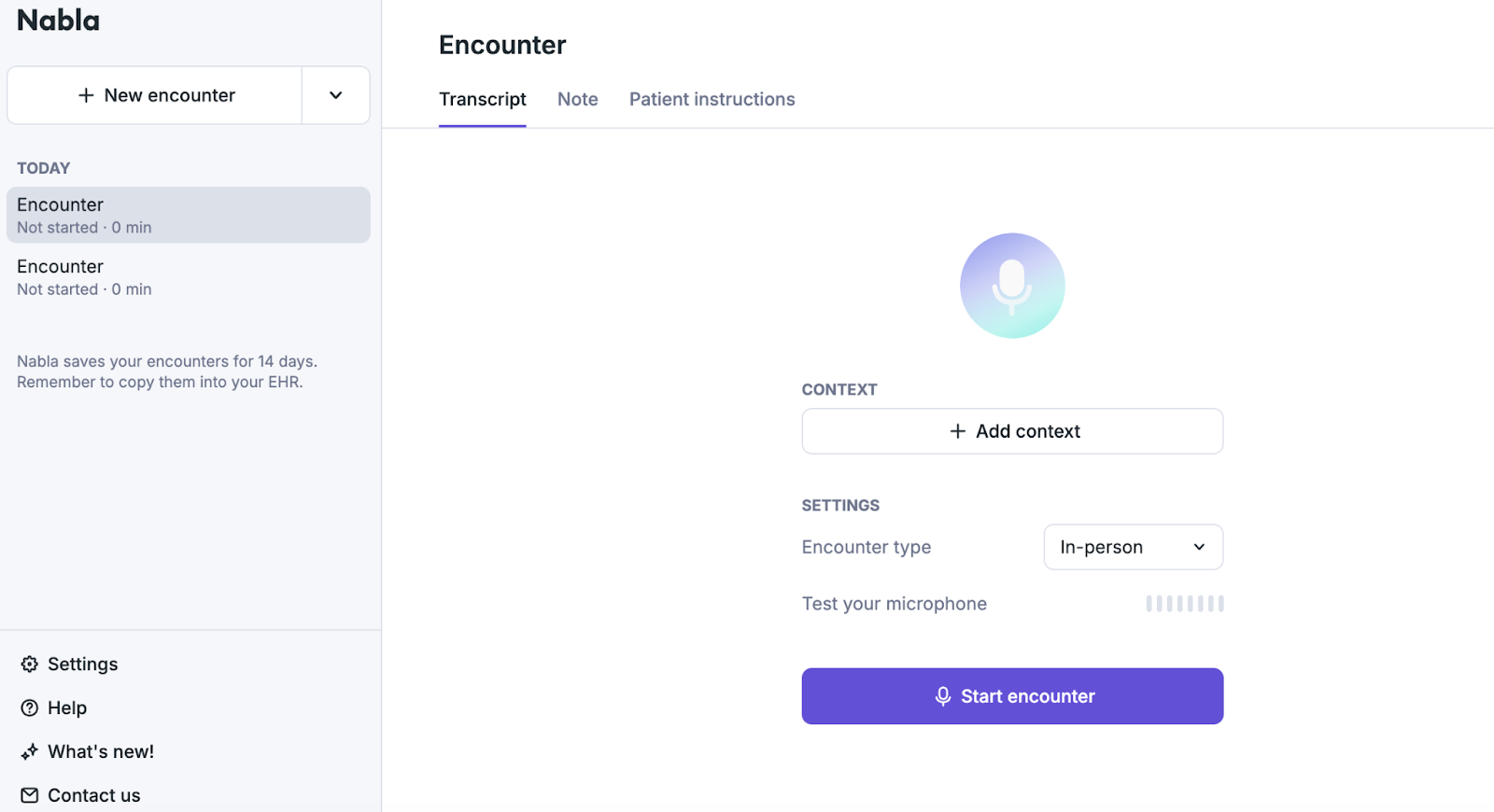
Nabla’s Copilot is a lightweight ambient assistant that listens during psychiatric visits and generates a draft note from the live conversation, with an on‑screen transcript that many trainees and early‑career clinicians find helpful for teaching and recall. It is best thought of as a “co‑pilot” that scaffolds HPI and assessment sections rather than a full psychiatry‑specific documentation system.
One reddit user notes, “Same vibe as Freed, clean UI, but felt bare-bones. If you want something super simple, it’ll do the trick, but I needed more control and accuracy. Lacks a lot of specialty/custom options.”
Best for
- Psychiatry residents, fellows, and PMHNPs who want a live transcript plus quick draft notes to structure HPIs and assessments
- Clinicians looking for a low‑friction, low‑commitment way to try ambient documentation in outpatient psychiatry
Not as great for
- Psychiatrists who need highly detailed, structured MSE and risk‑assessment language straight out of the box
- Complex psychotherapy or combined therapy‑plus‑med sessions where deep narrative nuance is essential
Pros
- Provides a live transcript during the encounter, which can support teaching, supervision, and immediate clarification
- One‑click note generation from the transcript helps reduce after‑visit typing for straightforward follow‑ups
- A relatively simple setup makes it accessible for clinicians experimenting with ambient AI without overhauling their workflow
Cons
- Drafts often require meaningful editing to accurately capture MSE, safety language, and nuanced psychopharmacology decisions
- Less tuned to long‑form psychotherapy content, so psychiatrists may still rely on manual narrative for complex visits
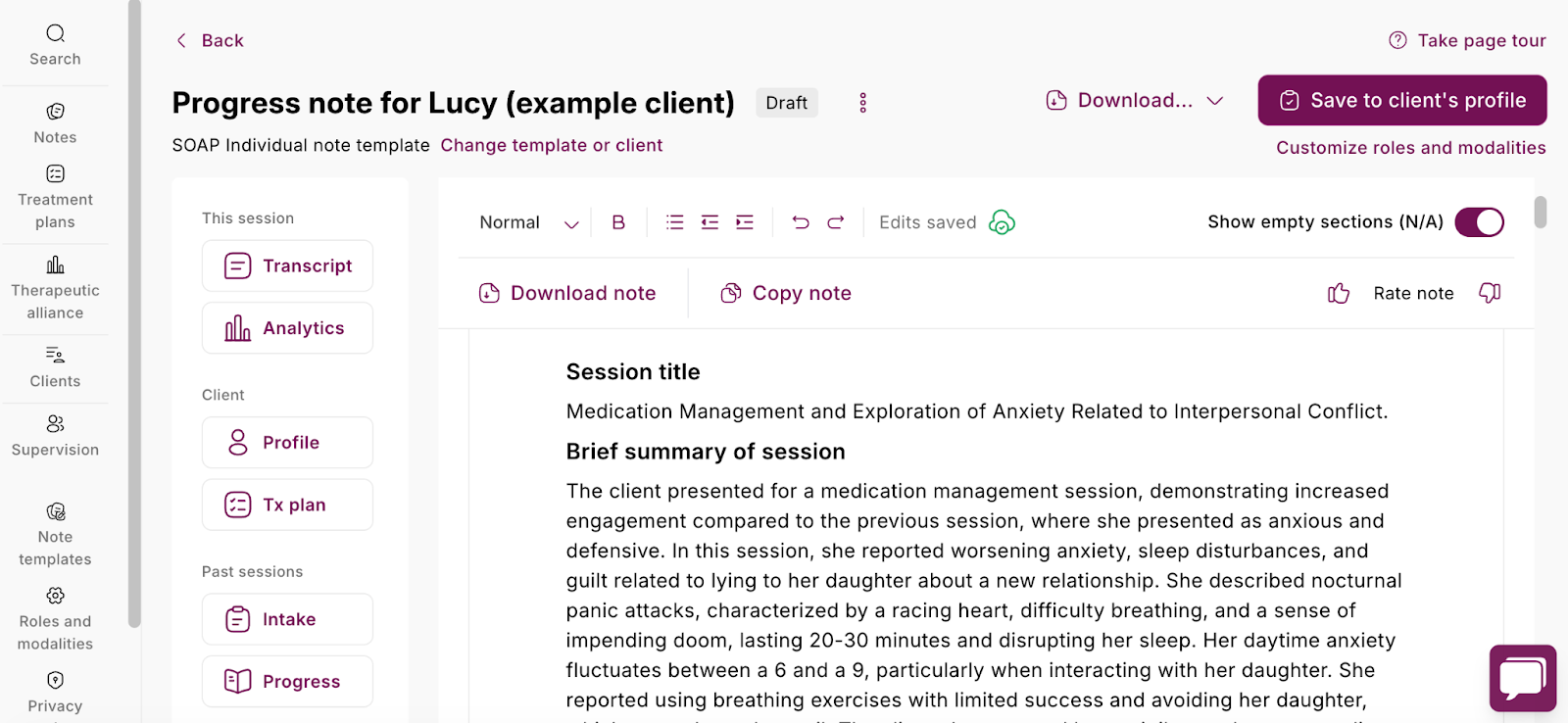
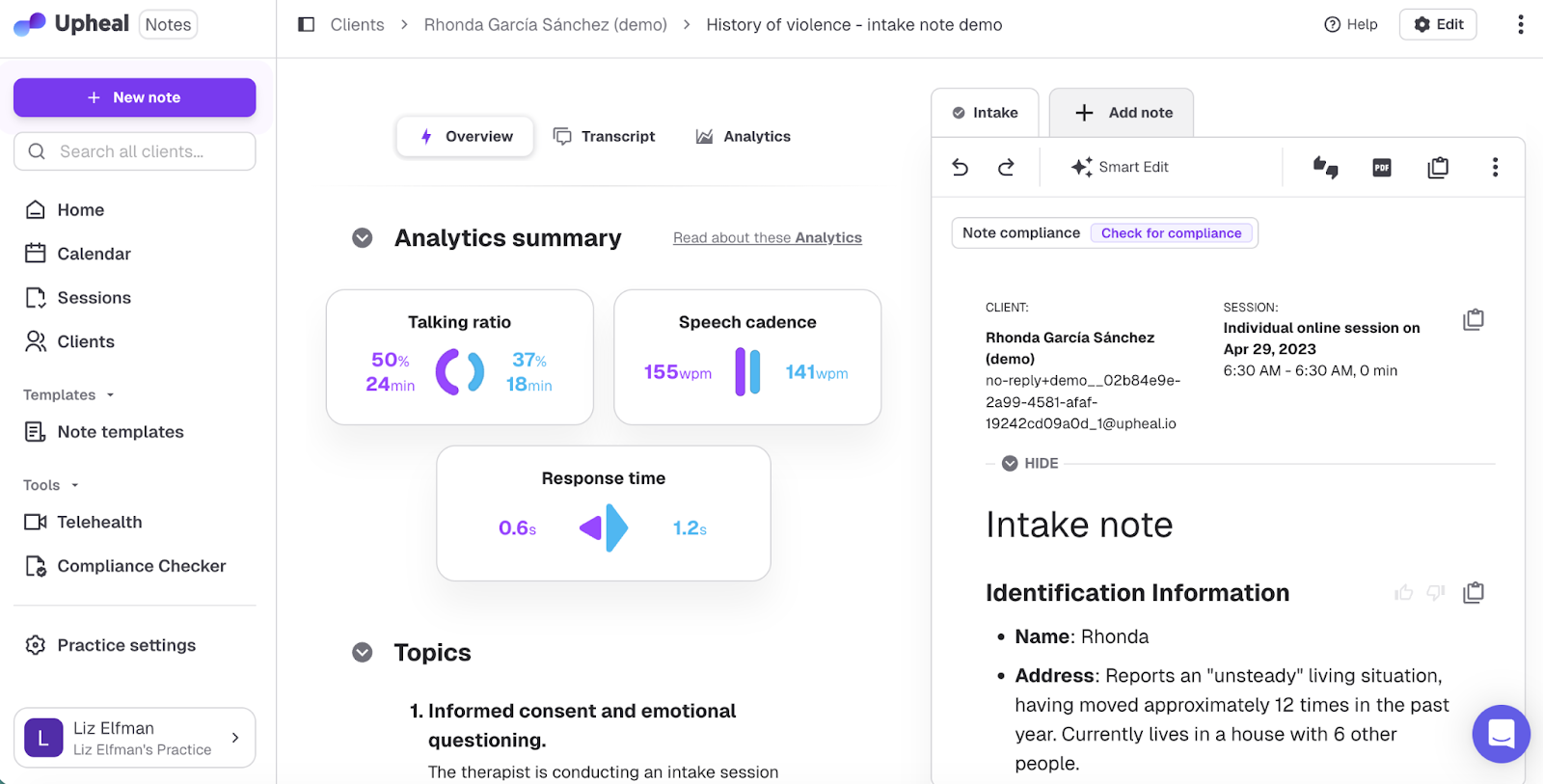
5. Upheal
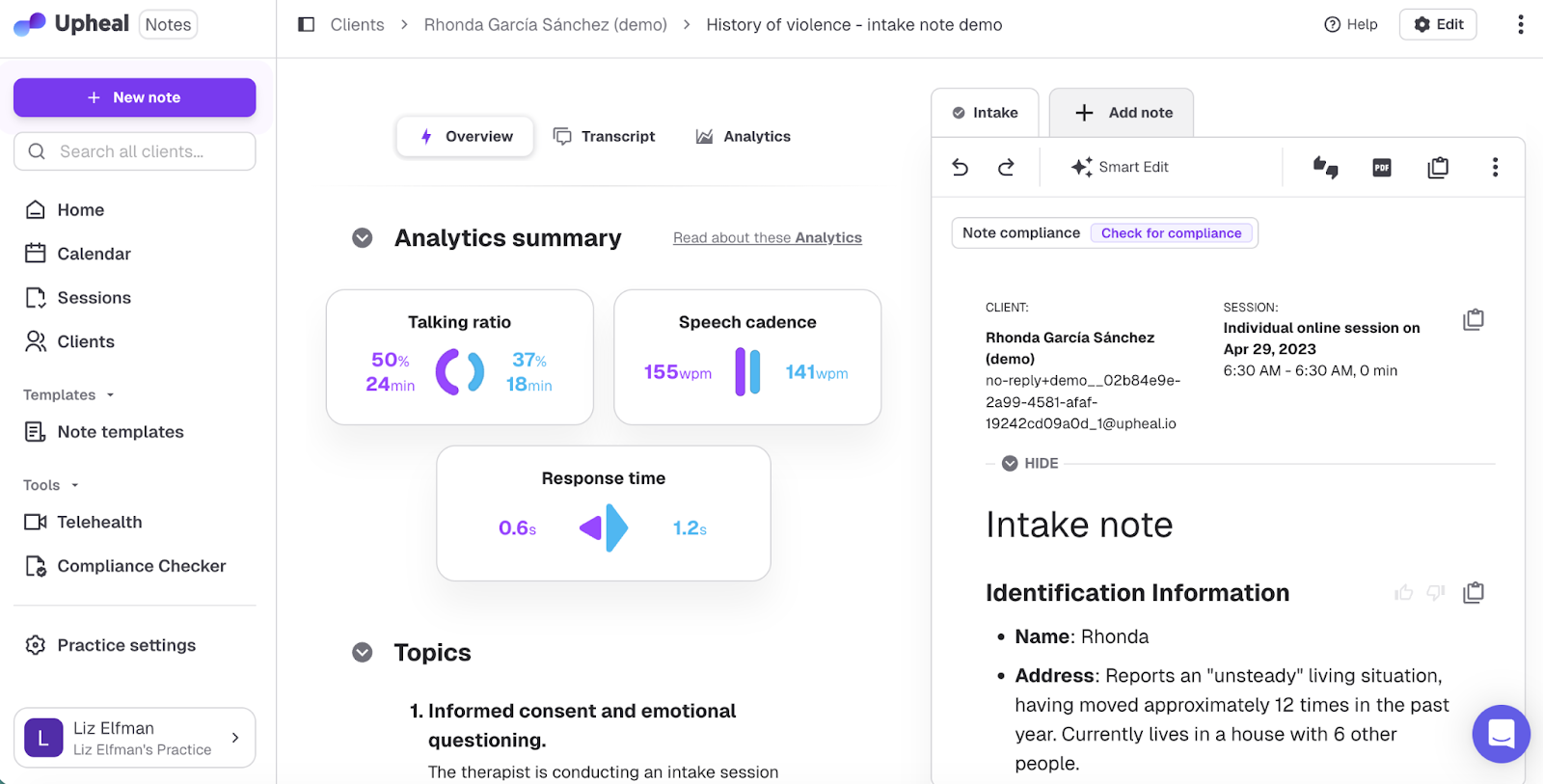
Upheal is an “all‑in‑one” platform that records psychiatry sessions with consent, generates transcripts, and exports SOAP/DAP/GIRP notes while also surfacing patterns in mood, themes, and goals over time. For many psychiatrists, it functions less like a simple scribe and more like a formulation and supervision aid for long‑term, psychotherapy‑heavy cases.
One Reddit clinician writes, “Upheal was very intuitive to use, the notes it put out were really well written and accurate to the discussion it recorded, or the notes I put in if the client didn’t want to record.”
Best for
- Psychiatrists and PMHNPs in group or training settings who want standardized documentation plus data to support QA, supervision, and case reviews
- Clinicians doing substantial psychotherapy alongside med management who value longitudinal insight into symptoms, themes, and treatment response
Not as great for
- Psychiatrists who do not want session audio or analytics stored in a vendor’s cloud under any circumstances, even with HIPAA/SOC 2 safeguards
- Providers who prefer the simplest possible “record and paste a note” experience without dashboards, analytics, or extra views
Pros
- Multi‑format exports (SOAP, DAP, GIRP) that align with psychotherapy and psychiatry documentation standards, including longer‑term treatment
- Built‑in consent flows that make it easier to handle recording ethically in psychiatric care, especially around sensitive content
- Analytics, goals, and insight views that can support formulation, supervision, and measurement‑based care over the course of treatment
Cons
- Audio and derived analytics are stored in the cloud, which some privacy‑focused psychiatrists avoid despite compliance assurances
- A more complex interface and higher bandwidth demands than lightweight, scribe‑only tools, which can feel heavy for short, med‑only visits
- and bandwidth demands can make it feel heavy compared with lighter note‑only tools
6. Mentalyc
Mentalyc is a privacy‑forward AI documentation tool, which makes it appealing for psychiatrists working with highly sensitive populations or forensic‑adjacent cases. It is built for mental‑health workflows rather than general medical documentation, with support for common psychotherapy note formats and export into existing EHRs.
One Reddit user notes, “After trying Mentalyc I was pleasantly surprised. It handles different note formats well and keeps things structured without feeling too generic. What stood out most was consistency — notes across sessions feel cleaner and easier to maintain. There’s a bit of a learning curve at first, but once you understand how to input sessions, it speeds things up a lot.”
Best for
- Psychiatrists and PMHNPs who treat high‑risk or highly sensitive patients and want anonymized transcripts plus strict control over what is stored
- Clinicians who are comfortable recording or uploading audio but prefer that raw recordings are not retained long term
Not as great for
- Providers who expect zero hallucinations or phrasing errors from AI output and are unwilling to review each note carefully before signing
- Clinicians who rely on fully offline workflows or need native mobile apps for field‑based or in‑home work, since Mentalyc is primarily browser‑based
Pros
- Strong privacy posture, including encrypted and anonymized transcriptions, HIPAA/PHIPA/SOC 2 compliance, and BAAs, with marketing explicitly focused on reducing note backlog and after‑hours charting
- Designed for mental health, with multiple note formats (SOAP, DAP, BIRP, PIRP, GIRP, SIRP, etc.), support for various modalities (CBT, DBT, EMDR, trauma‑focused work), and one‑click export into the EHR you already use
- Provides informed‑consent guidance and emphasizes that clinicians remain in control, reviewing AI‑generated drafts and using additional features like treatment planning and progress tracking as needed
Cons
- Some clinicians report that, while it significantly reduces time on notes, drafts still require review and occasional correction to ensure complete accuracy
- The browser‑based interface and rich feature set can feel heavier than minimalist scribe‑only tools for psychiatrists who just want a very simple “capture and paste” workflow
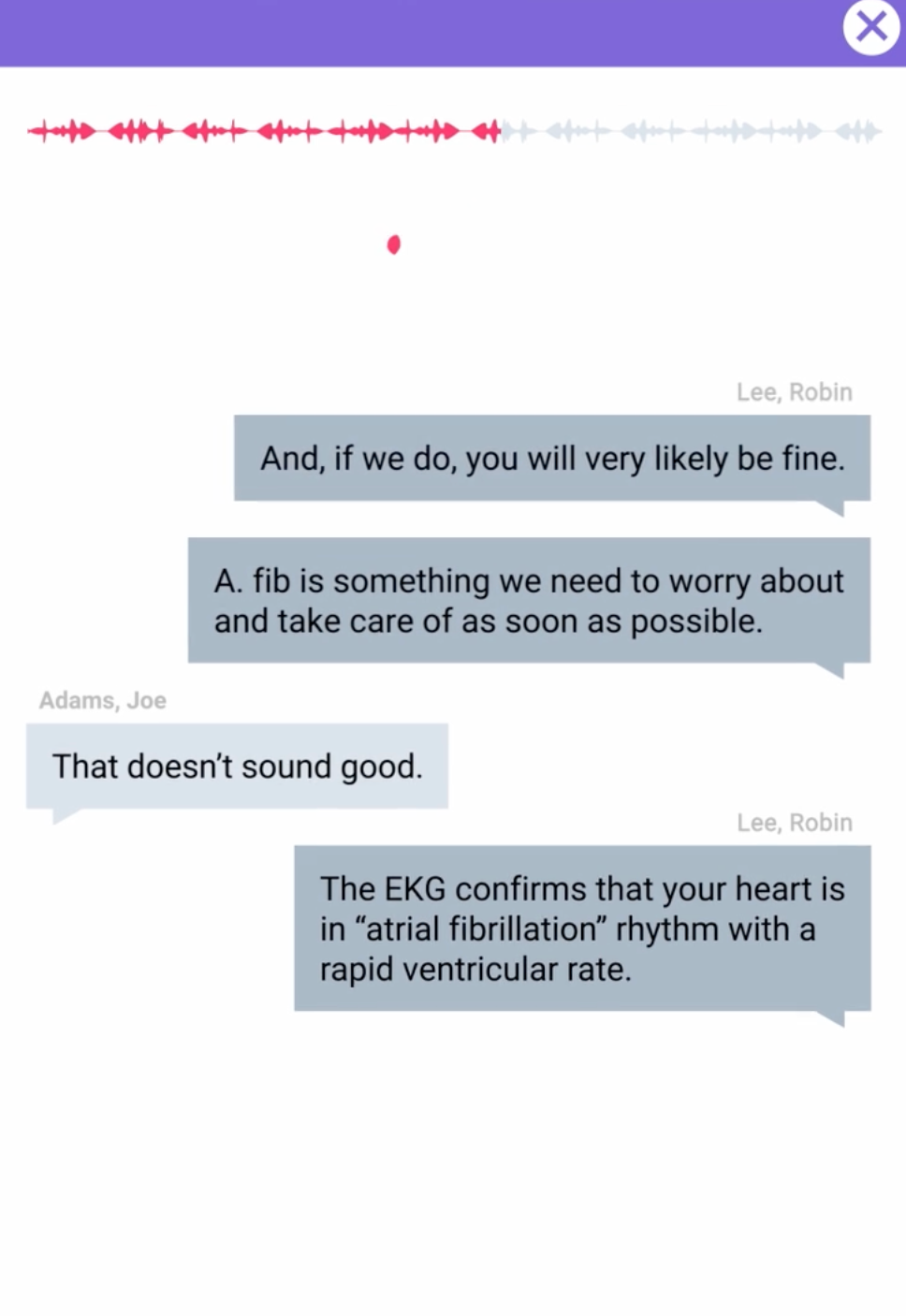
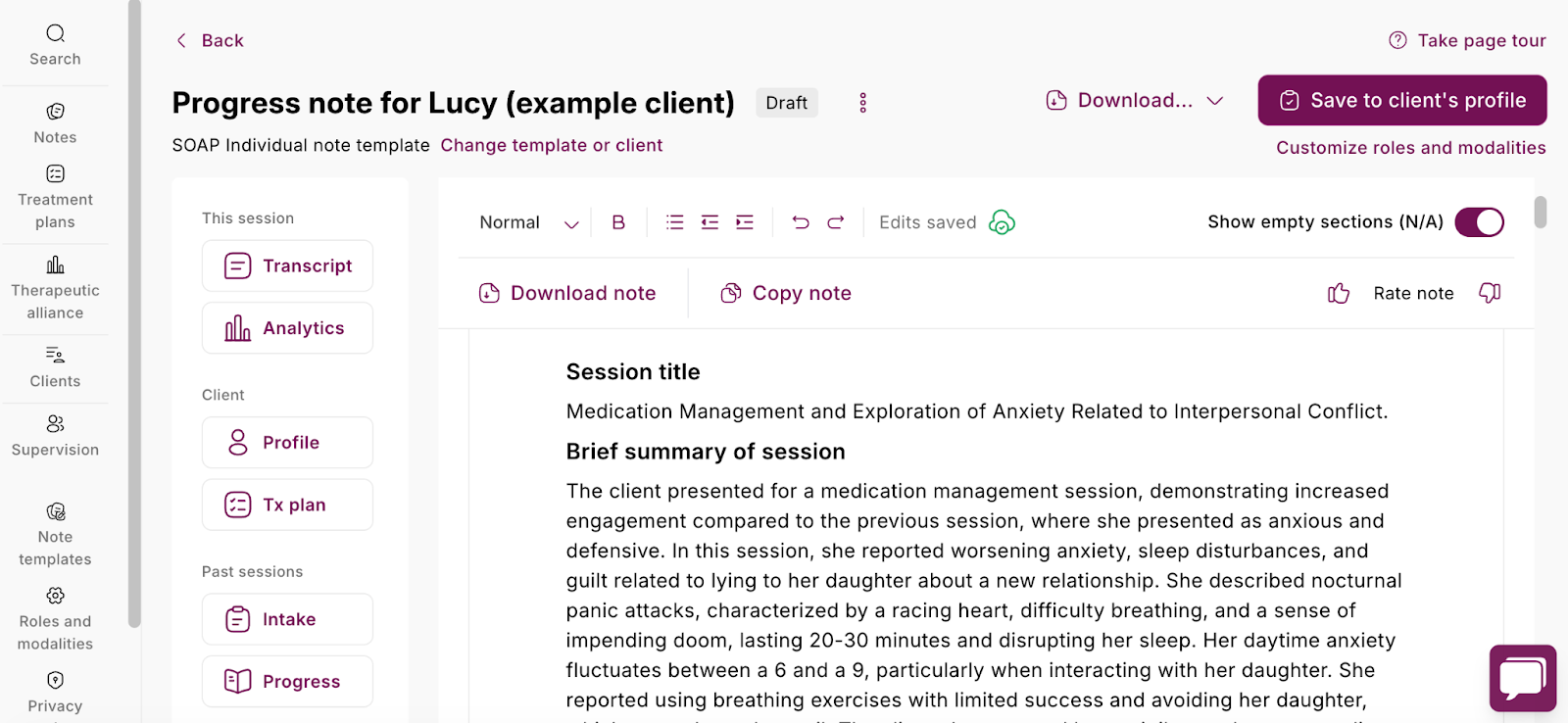
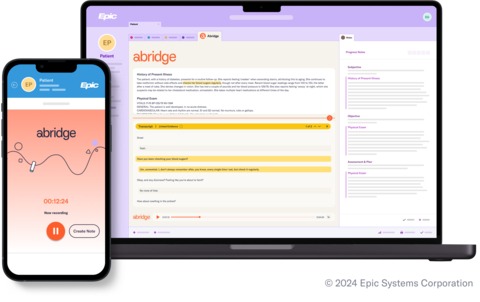
7. Abridge
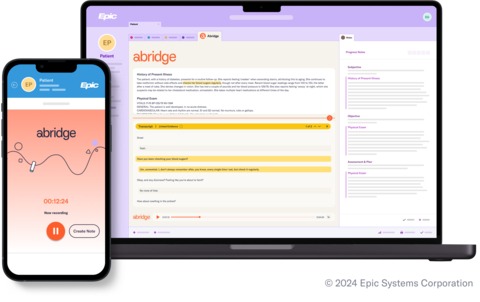
Abridge is widely deployed across medical specialties and increasingly adopted in psychiatry departments within large health systems, where visits blend medication management, psychotherapy, and integrated behavioral health. It provides real‑time ambient transcription and summarization that generates structured notes directly inside Epic and other enterprise EHRs, reducing after‑hours work by up to 86% according to system-wide reports.
One G2 user notes, “Great summary of encounters, comprehensive prose and good plan and patient summary.”
Best for
- Psychiatrists embedded in Epic‑heavy hospitals, academic centers, or integrated care systems where deep EHR workflows are non‑negotiable
- Teams needing one ambient tool to handle both medical encounters and psychiatric visits with seamless note delivery into the chart
Not as great for
- Solo or small‑group psychiatrists who do not need (or want) enterprise‑level IT onboarding and integration requirements
- Clinicians who prefer lightweight, EHR‑agnostic tools with simple record‑and‑paste workflows over complex system coupling
Pros
- Real‑time ambient capture that handles psychiatric details alongside general medical content
- Native Epic integration (from Haiku mobile to Hyperdrive) plus structured templates that cut double documentation and support quality metrics
- Enterprise‑grade security used by Mayo Clinic, Johns Hopkins, Kaiser, and Duke, with multilingual support across care settings
Cons
- Sold exclusively through health system contracts, making it inaccessible and overkill for independent practices
- Note language can feel more generic than specialty‑tuned, requiring psychiatrists to personalize MSE and psychotherapy sections
8. Sunoh.ai
Sunoh.ai is an ambient AI scribe tightly integrated with eClinicalWorks that has expanded into behavioral health and psychiatry, generating structured SOAP or DAP notes from live psychiatric visits directly inside the ECW interface. Psychiatrists using ECW appreciate how it handles HPI, med management, and basic therapy content without leaving their EHR, often cutting charting time significantly.
On Capterra, one clinician notes, “It cuts down on time and gives us more time to focus on the patient's needs. Fast, easy, and mobile! It makes the doctors schedule way faster, and they can even fit in more patients.”
Less favorable reviews were found on Reddit, with one user saying, “We use eClinicalWorks, Sunoh is built in, mostly good at picking up what is said and filters out what it thinks is not relevant. It doesn't capture who says what very well. It also is complete trash at anything beyond HPI.”
Best for
- Psychiatrists and PMHNPs standardized on eClinicalWorks who want ambient notes pushed directly into their existing charts
- Outpatient behavioral health teams doing med checks and structured follow-ups where ECW is already the workflow backbone
Not as great for
- Practices on non-ECW EHRs, as integration and optimization are built specifically around eClinicalWorks
- Complex psychotherapy sessions requiring nuanced MSE language, multi-speaker separation, or heavy narrative formulation
Pros
- ECW-native ambient listening with behavioral health templates that generate psychiatry-ready notes without copy-paste
- Usage-based pricing appeals to variable-caseload psychiatrists, with reviewers noting better HPI structure and faster chart completion
- Handles medication names, dosages, and common psychopharmacology discussions accurately for med-management visits
Cons
- Reviews mention inconsistent speaker attribution and weaker handling of assessment/plan sections beyond basic HPI.
- Locked to eClinicalWorks ecosystem, limiting appeal if your practice might switch EHRs or needs broad compatibility.
9. Suki AI
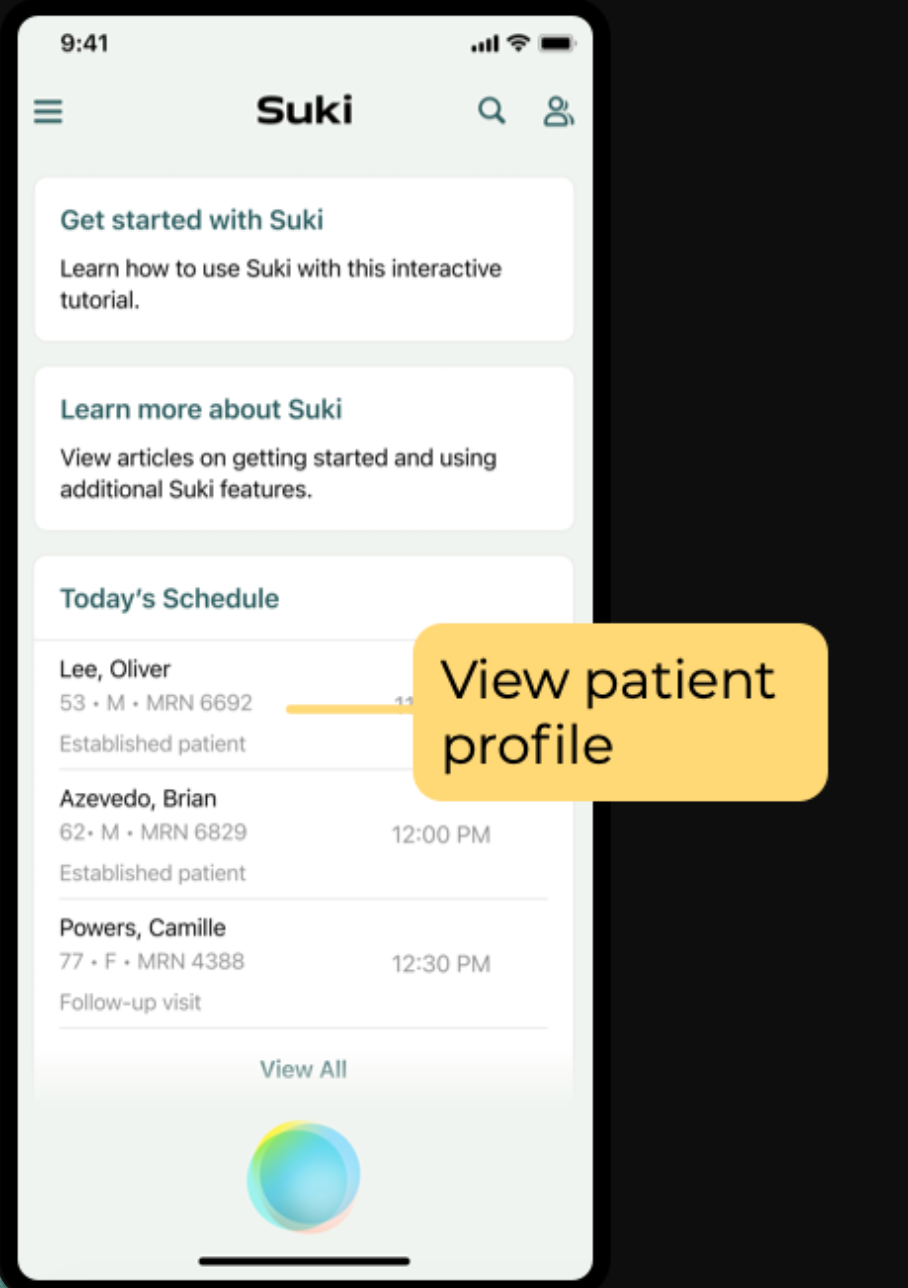
Suki AI combines voice commands with ambient assistance, making it a strong fit for psychiatrists whose visits center on medication management, ICD coding, and structured follow-ups rather than extended psychotherapy. Psychiatrists value how it lets them dictate orders, pull up templates, and generate note sections hands-free while staying focused on the patient.
Best for
- Outpatient psychiatrists with med-heavy caseloads who want voice-driven control over diagnoses, prescriptions, and plan sections
- Clinics already using major EHRs where Suki's voice commands can reduce clicks across documentation and ordering workflows
Not as great for
- Psychotherapy-focused visits needing rich narrative MSE descriptions or complex therapeutic process notes
- Psychiatrists who prefer fully passive ambient listening over active voice interaction during sessions
Pros
- Voice commands streamline medication orders, ICD-10 coding, and structured note sections, cutting documentation time for med checks
- Strong EHR connectivity across major platforms, reducing manual entry for multi-specialty or integrated behavioral health teams
- Adapts to clinician voice patterns and preferences, improving accuracy for frequent psychopharmacology terms
Cons
- Less optimized for psychotherapy nuance or extended patient narratives compared to therapy-first tools
- Requires initial customization and voice training, which adds setup time before full efficiency
How to choose the best AI scribe for psychiatry
Psychiatrists usually decide between AI scribes based on three things: comfort with recording, tolerance for editing, and how closely they want the scribe tied to their EHR. Evidence on ambient documentation suggests these choices affect not only convenience but also burnout and perceived documentation quality.
For many psychiatrists:
- If you want strong notes from live psychiatric conversations without changing EHRs, Freed offers ambient‑style capture with flexible EHR-push or “paste anywhere” output that works across all web‑based systems.
- If privacy is your top concern, therapy‑first platforms like Mentalyc emphasize anonymized transcripts, minimal audio retention, and clear policies around recording and subpoenas.
- If you work inside a health system, enterprise options such as Abridge or DAX integrate directly into the EHR and mirror the ambient documentation models evaluated in recent studies, but are often unavailable to independent psychiatrists.
The best AI scribe for your particular psychiatric practice is the one that actually gets you out of the clinic on time, preserves your confidence in what you sign, and aligns with the privacy commitments you make to patients.
Ready to see what an AI scribe can do for your psychiatry practice?
AI scribes won't replace the clinical judgment that defines psychiatric care, but they can give you back the time and presence that documentation has quietly stolen.
Whether you're managing complex medication regimens, navigating high-acuity crises, or balancing therapy with prescribing, the right AI scribe should feel less like another system to manage and more like the professional support you'd hire if you could.
The tools reviewed here represent real options for real psychiatric workflows — each with trade-offs integration, editing burden, and cost. The psychiatrists who benefit most are the ones who choose thoughtfully, pilot carefully, and remain the final authority on every note they sign.
If ambient documentation can cut your after-hours charting by even 30%, that's sustainability.
Ready to reclaim your evenings and stay present with patients? Try Freed for free.
Table of Contents
No matter the visit or client, charting eats our time. Between medication management, progress notes, and therapy portions of visits, it’s easy to lose another hour to documentation after-clinic.
AI scribes have matured quickly since 2024. A 2025 JAMA Network Open study found ambient documentation tools reduced clinician after-hours charting by 41% and improved professional fulfillment scores by 53%—with even greater gains in high-documentation specialties like psych.
Today’s psychiatry‑friendly platforms can:
- Listen to your in-person or telehealth sessions
- Summarize the essential clinical points
- Draft a note that respects both HIPAA and your personal documentation style.
Below is a psychiatry‑focused comparison of leading AI scribe tools as of 2026, based on firsthand clinician reviews on Reddit, G2, and other internet platforms.
Best AI scribes for psychiatrists, at a glance
How we evaluated AI scribes for psychiatrists
This roundup was built around how AI scribes perform in real psychiatric practice, not how they look in a sales deck. For each tool, the evaluation centered on:
- What psychiatrists, residents, and PMHNPs report about day‑to‑day use in clinic, including where tools actually save time and where they get in the way. These findings align with Mass General Brigham's 2025 analysis showing 78% of clinicians using ambient scribes reported less cognitive burden during visits.
- How well notes capture psychiatry‑specific elements: MSE, risk and safety language, psychotherapy themes, and medication rationale—not just a generic HPI.
- The editing load before a note is safe to sign and bill, especially for complex follow‑ups and crisis visits.
Platform fit also mattered:
- Whether the scribe works for common psychiatry setups (solo outpatient, group practices, community mental health, and hospital‑based services).
- How tightly it is tied to a single EHR versus flexible enough to follow psychiatrists across roles or organizations.
- Its stance on privacy and consent in mental health settings, including how recordings and transcripts are handled over time.
The aim was not to name one “best” product, but to map the trade‑offs psychiatrists actually face when choosing AI scribes that reduce documentation burden while still supporting sound clinical judgment.
What is an AI scribe for psychiatrists?
AI scribes for psychiatry turn visits into draft clinical notes — covering HPI, MSE, risk assessment, and treatment plan—using conversation, dictation, or structured input. They cut after-hours charting while keeping notes clinically sound and billable.
Psychiatry tools fall into four main types:
Ambient AI scribes
Listen live (in-person/telepsychiatry) to generate drafts from dialogue, reducing memory reconstruction of MSE or risk language. Freed and Abridge are examples.
Dictation-based tools
Post-visit verbal summary becomes structured SOAP/DAP notes. TherapyNotes AI and similar tools require recall but beat typing.
Prompt-based tools
Type key points (symptoms, meds, plan) for instant note drafts. Best for organized med-checks, less helpful during complex visits.
Measurement-driven tools
Use PHQ-9/GAD-7 scores plus text for progress notes tied to outcomes. Blueprint fits insurance-heavy psychiatry but limits narrative.
AI scribe options for psychiatrists
1. Freed
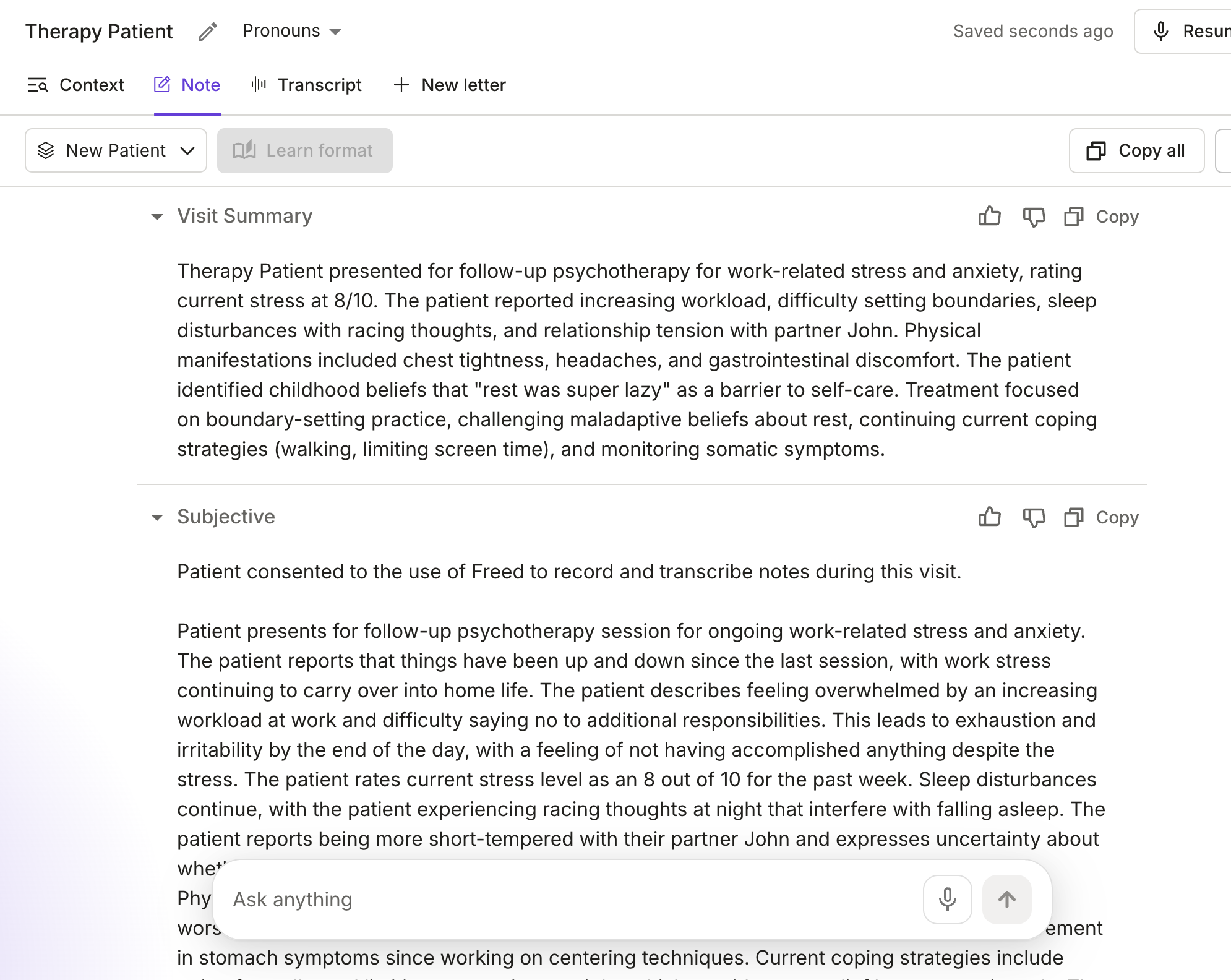
Freed is an ambient AI medical scribe designed to handle the realities of psychiatric visits — long conversations, nuanced mental status exams, medication management, and sensitive risk language — without forcing you to change how you practice or which EHR you use. The tool is HIPAA and HITECH compliant with industry-leading security standards.
Clinicians on Reddit describe Freed as follows: “the note this thing generated was precise, comprehensive, well-written and actually sounded like me. I was blown away. It would have taken me an easy 30 minutes to write a similar note.”
Freed listens to in‑person or telepsychiatry encounters and turns the conversation into clean narrative or SOAP‑style, customizable notes you can drop into virtually any web‑based EHR.
Freed’s EHR push feature allows a one-click push to any web-based EHR through its Chrome Extension, including Simple Practice, PracticeFusion, Athena Health and more.
One psychiatric clinician writes, “I was getting burned out, but that all changed with Freed. Now visits feel like I have a personal scribe in the background capturing every detail, freeing me to be 100% present with my patients. It’s far more efficient to review and edit a note already structured in SOAP format than write one from memory. I’ve been freed!”
Best for
- Psychiatrists and PMHNPs who want strong HPI, MSE, and plan drafts from live visits without switching EHRs
- Clinicians who prefer flat, predictable monthly pricing over per‑minute audio charges
Not as great for
- Larger hospital organizations
Pros
- Customizable templates that learn from your edits
- Advanced features like smart visit prep and patient letters, referrals, and more
- HIPAA‑compliant with BAAs on paid plans
- Paragraph‑style notes that often need only light editing, according to multiple Reddit and G2 reviewers
- Works across devices and fits with workflows like Zoom, so you can use it for both in‑person and telehealth sessions
Cons
- Free trial lasts only 7 days, no permanent free tier
2. TherapyNotes AI
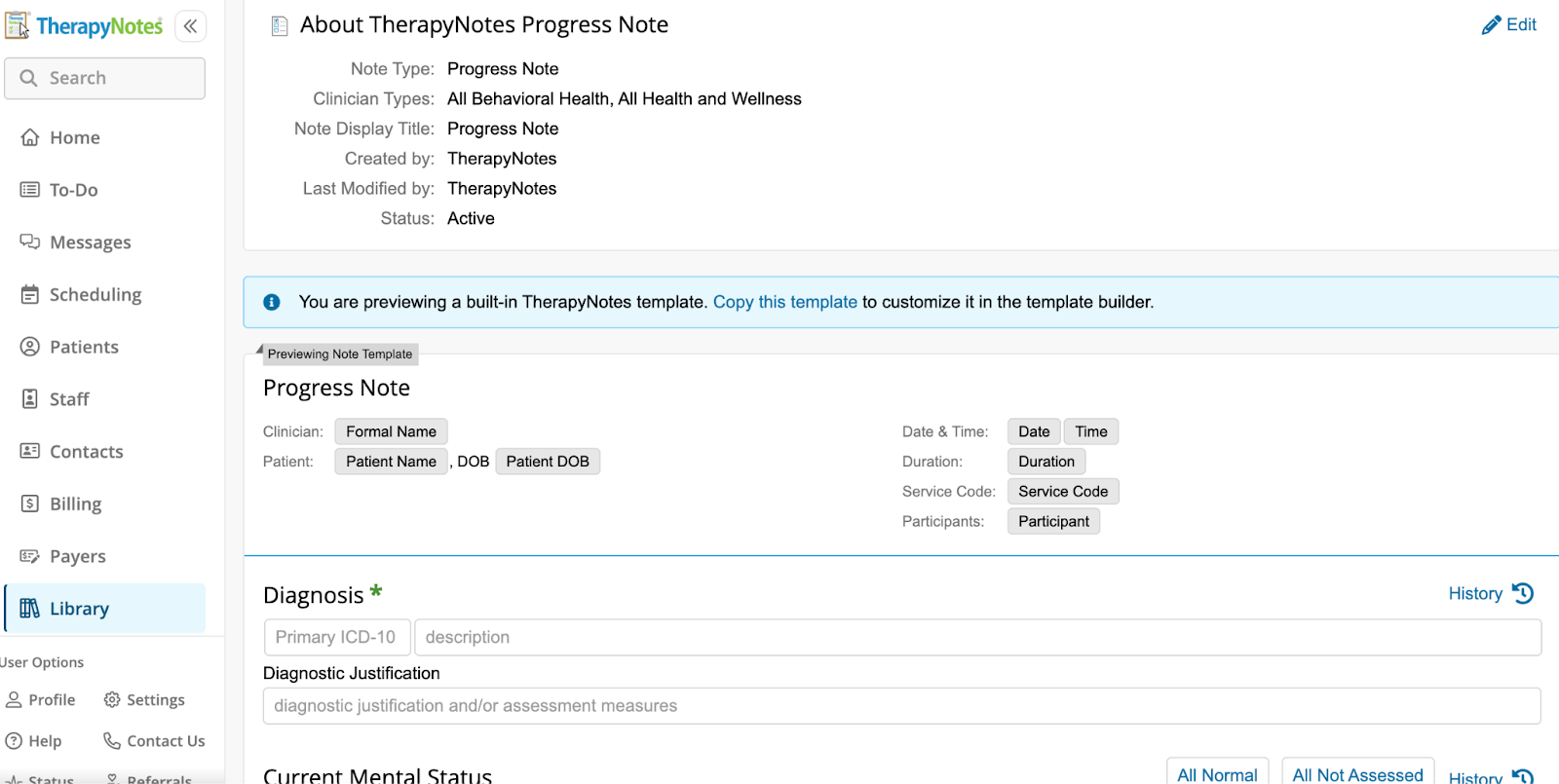
Many psychiatrists rely on TherapyNotes for scheduling, billing, and documentation. Its AI TherapyFuel functionality gives those users a built-in way to generate note drafts through AI, within the same EHR. It takes dictation or typed summaries and produces SOAP or DAP‑style notes directly.
One reddit user notes, “It definitely has some flaws, but it has made documentation much easier. It has helped me to stay more on top of note taking. I always read through and edit as necessary, but it does well.”
Best for
- Psychiatric practitioners who already use TherapyNotes and want AI support without adding another standalone tool
- Practices that prefer to keep billing, documentation, and AI‑generated drafts inside a single HIPAA‑compliant platform
Not as great for
- Clinicians using other EHRs or non‑EHR workflows, since the AI is not available as a separate product
- Psychiatrists who want highly nuanced, specialty‑tuned language for complex MSEs or psychodynamic notes rather than more generic drafts
Pros
- Embedded directly in TherapyNotes, avoiding copy‑and‑paste and keeping everything in one system
- Supports common mental‑health formats like SOAP and DAP for both therapy and med‑management visits
- Includes AI settings and consent language in the same place you manage the rest of your notes
Cons
- Independent reviews characterize it as “good but generic,” meaning you still need to refine tone and nuance
- Available only inside TherapyNotes, so you cannot use it if your practice runs on other platforms
3. Blueprint
Blueprint is not a traditional ambient scribe, but it uses standardized outcome measures (like PHQ‑9, GAD‑7, and related scales) plus brief text to generate structured progress notes and track symptom change over time in psychiatric care. That makes it especially appealing in insurance‑heavy, measurement‑based psychiatry, where tying documentation to validated instruments is a constant ask.
One Reddit user notes, “I use Blueprint and I love it. It’s HIPAA compliant, doesn’t sell the info, is a private company….It simply organizes my thoughts in a way that’s more coherent. You can add or delete as you wish and you should definitely read everything it generates from your notes to be sure it’s correct.”
Best for
- Psychiatrists and PMHNPs in clinics where payers expect regular use of validated scales and formal measurement‑based care
- Practices that want dashboards showing symptom trajectories, engagement, and outcomes alongside their notes
Not as great for
- Private‑pay or boutique practices where measurement scales are used infrequently
- Psychiatrists who prefer free‑form, psychodynamic‑style notes and rich process descriptions rather than scale‑anchored language
Pros
- Builds notes from rating‑scale data plus text, clearly linking documentation to treatment goals, severity, and outcomes for audits and payers
- Offers progress charts and other measurement‑based care tools that help visualize change over time
- Integrates with some EHRs, reducing manual efforts
Cons
- Note language can feel constrained by the underlying scales and may not capture nuanced psychodynamics or complex interpersonal themes
- Per‑client or per‑use pricing can add up for psychiatrists managing large, high‑acuity caseloads
4. Nabla
Nabla’s Copilot is a lightweight ambient assistant that listens during psychiatric visits and generates a draft note from the live conversation, with an on‑screen transcript that many trainees and early‑career clinicians find helpful for teaching and recall. It is best thought of as a “co‑pilot” that scaffolds HPI and assessment sections rather than a full psychiatry‑specific documentation system.
One reddit user notes, “Same vibe as Freed, clean UI, but felt bare-bones. If you want something super simple, it’ll do the trick, but I needed more control and accuracy. Lacks a lot of specialty/custom options.”
Best for
- Psychiatry residents, fellows, and PMHNPs who want a live transcript plus quick draft notes to structure HPIs and assessments
- Clinicians looking for a low‑friction, low‑commitment way to try ambient documentation in outpatient psychiatry
Not as great for
- Psychiatrists who need highly detailed, structured MSE and risk‑assessment language straight out of the box
- Complex psychotherapy or combined therapy‑plus‑med sessions where deep narrative nuance is essential
Pros
- Provides a live transcript during the encounter, which can support teaching, supervision, and immediate clarification
- One‑click note generation from the transcript helps reduce after‑visit typing for straightforward follow‑ups
- A relatively simple setup makes it accessible for clinicians experimenting with ambient AI without overhauling their workflow
Cons
- Drafts often require meaningful editing to accurately capture MSE, safety language, and nuanced psychopharmacology decisions
- Less tuned to long‑form psychotherapy content, so psychiatrists may still rely on manual narrative for complex visits
5. Upheal
Upheal is an “all‑in‑one” platform that records psychiatry sessions with consent, generates transcripts, and exports SOAP/DAP/GIRP notes while also surfacing patterns in mood, themes, and goals over time. For many psychiatrists, it functions less like a simple scribe and more like a formulation and supervision aid for long‑term, psychotherapy‑heavy cases.
One Reddit clinician writes, “Upheal was very intuitive to use, the notes it put out were really well written and accurate to the discussion it recorded, or the notes I put in if the client didn’t want to record.”
Best for
- Psychiatrists and PMHNPs in group or training settings who want standardized documentation plus data to support QA, supervision, and case reviews
- Clinicians doing substantial psychotherapy alongside med management who value longitudinal insight into symptoms, themes, and treatment response
Not as great for
- Psychiatrists who do not want session audio or analytics stored in a vendor’s cloud under any circumstances, even with HIPAA/SOC 2 safeguards
- Providers who prefer the simplest possible “record and paste a note” experience without dashboards, analytics, or extra views
Pros
- Multi‑format exports (SOAP, DAP, GIRP) that align with psychotherapy and psychiatry documentation standards, including longer‑term treatment
- Built‑in consent flows that make it easier to handle recording ethically in psychiatric care, especially around sensitive content
- Analytics, goals, and insight views that can support formulation, supervision, and measurement‑based care over the course of treatment
Cons
- Audio and derived analytics are stored in the cloud, which some privacy‑focused psychiatrists avoid despite compliance assurances
- A more complex interface and higher bandwidth demands than lightweight, scribe‑only tools, which can feel heavy for short, med‑only visits
- and bandwidth demands can make it feel heavy compared with lighter note‑only tools
6. Mentalyc
Mentalyc is a privacy‑forward AI documentation tool, which makes it appealing for psychiatrists working with highly sensitive populations or forensic‑adjacent cases. It is built for mental‑health workflows rather than general medical documentation, with support for common psychotherapy note formats and export into existing EHRs.
One Reddit user notes, “After trying Mentalyc I was pleasantly surprised. It handles different note formats well and keeps things structured without feeling too generic. What stood out most was consistency — notes across sessions feel cleaner and easier to maintain. There’s a bit of a learning curve at first, but once you understand how to input sessions, it speeds things up a lot.”
Best for
- Psychiatrists and PMHNPs who treat high‑risk or highly sensitive patients and want anonymized transcripts plus strict control over what is stored
- Clinicians who are comfortable recording or uploading audio but prefer that raw recordings are not retained long term
Not as great for
- Providers who expect zero hallucinations or phrasing errors from AI output and are unwilling to review each note carefully before signing
- Clinicians who rely on fully offline workflows or need native mobile apps for field‑based or in‑home work, since Mentalyc is primarily browser‑based
Pros
- Strong privacy posture, including encrypted and anonymized transcriptions, HIPAA/PHIPA/SOC 2 compliance, and BAAs, with marketing explicitly focused on reducing note backlog and after‑hours charting
- Designed for mental health, with multiple note formats (SOAP, DAP, BIRP, PIRP, GIRP, SIRP, etc.), support for various modalities (CBT, DBT, EMDR, trauma‑focused work), and one‑click export into the EHR you already use
- Provides informed‑consent guidance and emphasizes that clinicians remain in control, reviewing AI‑generated drafts and using additional features like treatment planning and progress tracking as needed
Cons
- Some clinicians report that, while it significantly reduces time on notes, drafts still require review and occasional correction to ensure complete accuracy
- The browser‑based interface and rich feature set can feel heavier than minimalist scribe‑only tools for psychiatrists who just want a very simple “capture and paste” workflow
7. Abridge
Abridge is widely deployed across medical specialties and increasingly adopted in psychiatry departments within large health systems, where visits blend medication management, psychotherapy, and integrated behavioral health. It provides real‑time ambient transcription and summarization that generates structured notes directly inside Epic and other enterprise EHRs, reducing after‑hours work by up to 86% according to system-wide reports.
One G2 user notes, “Great summary of encounters, comprehensive prose and good plan and patient summary.”
Best for
- Psychiatrists embedded in Epic‑heavy hospitals, academic centers, or integrated care systems where deep EHR workflows are non‑negotiable
- Teams needing one ambient tool to handle both medical encounters and psychiatric visits with seamless note delivery into the chart
Not as great for
- Solo or small‑group psychiatrists who do not need (or want) enterprise‑level IT onboarding and integration requirements
- Clinicians who prefer lightweight, EHR‑agnostic tools with simple record‑and‑paste workflows over complex system coupling
Pros
- Real‑time ambient capture that handles psychiatric details alongside general medical content
- Native Epic integration (from Haiku mobile to Hyperdrive) plus structured templates that cut double documentation and support quality metrics
- Enterprise‑grade security used by Mayo Clinic, Johns Hopkins, Kaiser, and Duke, with multilingual support across care settings
Cons
- Sold exclusively through health system contracts, making it inaccessible and overkill for independent practices
- Note language can feel more generic than specialty‑tuned, requiring psychiatrists to personalize MSE and psychotherapy sections
8. Sunoh.ai
Sunoh.ai is an ambient AI scribe tightly integrated with eClinicalWorks that has expanded into behavioral health and psychiatry, generating structured SOAP or DAP notes from live psychiatric visits directly inside the ECW interface. Psychiatrists using ECW appreciate how it handles HPI, med management, and basic therapy content without leaving their EHR, often cutting charting time significantly.
On Capterra, one clinician notes, “It cuts down on time and gives us more time to focus on the patient's needs. Fast, easy, and mobile! It makes the doctors schedule way faster, and they can even fit in more patients.”
Less favorable reviews were found on Reddit, with one user saying, “We use eClinicalWorks, Sunoh is built in, mostly good at picking up what is said and filters out what it thinks is not relevant. It doesn't capture who says what very well. It also is complete trash at anything beyond HPI.”
Best for
- Psychiatrists and PMHNPs standardized on eClinicalWorks who want ambient notes pushed directly into their existing charts
- Outpatient behavioral health teams doing med checks and structured follow-ups where ECW is already the workflow backbone
Not as great for
- Practices on non-ECW EHRs, as integration and optimization are built specifically around eClinicalWorks
- Complex psychotherapy sessions requiring nuanced MSE language, multi-speaker separation, or heavy narrative formulation
Pros
- ECW-native ambient listening with behavioral health templates that generate psychiatry-ready notes without copy-paste
- Usage-based pricing appeals to variable-caseload psychiatrists, with reviewers noting better HPI structure and faster chart completion
- Handles medication names, dosages, and common psychopharmacology discussions accurately for med-management visits
Cons
- Reviews mention inconsistent speaker attribution and weaker handling of assessment/plan sections beyond basic HPI.
- Locked to eClinicalWorks ecosystem, limiting appeal if your practice might switch EHRs or needs broad compatibility.
9. Suki AI
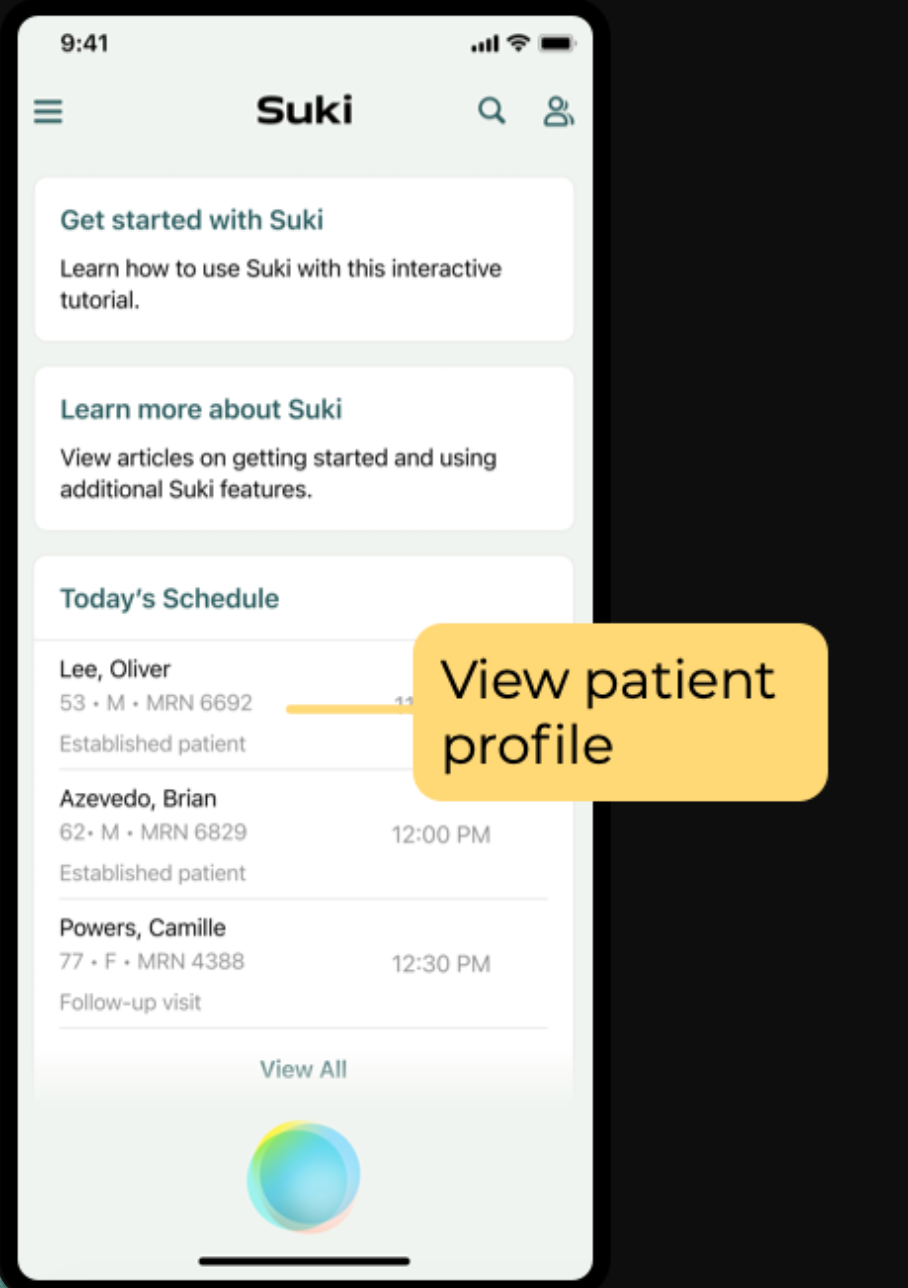
Suki AI combines voice commands with ambient assistance, making it a strong fit for psychiatrists whose visits center on medication management, ICD coding, and structured follow-ups rather than extended psychotherapy. Psychiatrists value how it lets them dictate orders, pull up templates, and generate note sections hands-free while staying focused on the patient.
Best for
- Outpatient psychiatrists with med-heavy caseloads who want voice-driven control over diagnoses, prescriptions, and plan sections
- Clinics already using major EHRs where Suki's voice commands can reduce clicks across documentation and ordering workflows
Not as great for
- Psychotherapy-focused visits needing rich narrative MSE descriptions or complex therapeutic process notes
- Psychiatrists who prefer fully passive ambient listening over active voice interaction during sessions
Pros
- Voice commands streamline medication orders, ICD-10 coding, and structured note sections, cutting documentation time for med checks
- Strong EHR connectivity across major platforms, reducing manual entry for multi-specialty or integrated behavioral health teams
- Adapts to clinician voice patterns and preferences, improving accuracy for frequent psychopharmacology terms
Cons
- Less optimized for psychotherapy nuance or extended patient narratives compared to therapy-first tools
- Requires initial customization and voice training, which adds setup time before full efficiency
How to choose the best AI scribe for psychiatry
Psychiatrists usually decide between AI scribes based on three things: comfort with recording, tolerance for editing, and how closely they want the scribe tied to their EHR. Evidence on ambient documentation suggests these choices affect not only convenience but also burnout and perceived documentation quality.
For many psychiatrists:
- If you want strong notes from live psychiatric conversations without changing EHRs, Freed offers ambient‑style capture with flexible EHR-push or “paste anywhere” output that works across all web‑based systems.
- If privacy is your top concern, therapy‑first platforms like Mentalyc emphasize anonymized transcripts, minimal audio retention, and clear policies around recording and subpoenas.
- If you work inside a health system, enterprise options such as Abridge or DAX integrate directly into the EHR and mirror the ambient documentation models evaluated in recent studies, but are often unavailable to independent psychiatrists.
The best AI scribe for your particular psychiatric practice is the one that actually gets you out of the clinic on time, preserves your confidence in what you sign, and aligns with the privacy commitments you make to patients.
Ready to see what an AI scribe can do for your psychiatry practice?
AI scribes won't replace the clinical judgment that defines psychiatric care, but they can give you back the time and presence that documentation has quietly stolen.
Whether you're managing complex medication regimens, navigating high-acuity crises, or balancing therapy with prescribing, the right AI scribe should feel less like another system to manage and more like the professional support you'd hire if you could.
The tools reviewed here represent real options for real psychiatric workflows — each with trade-offs integration, editing burden, and cost. The psychiatrists who benefit most are the ones who choose thoughtfully, pilot carefully, and remain the final authority on every note they sign.
If ambient documentation can cut your after-hours charting by even 30%, that's sustainability.
Ready to reclaim your evenings and stay present with patients? Try Freed for free.
FAQs
Frequently asked questions from clinicians and medical practitioners.
How do mental health professionals like psychiatrists, psychologists, and licensed social workers use SOAP note generators?
Is Freed secure and compliant with healthcare rules and regulations?
How can I get started with Freed?
How to write a good psychiatry note?
Related content






