The Future of Small Practices: How AI is Keeping Local Care Alive

The Future of Small Practices: How AI is Keeping Local Care Alive
AI isn’t a future fix. It’s already helping independent practices stay open, sane, and focused on care.
Table of Contents
For centuries, independent practices were the quiet backbone of American healthcare.
Your doctor wasn’t just your doctor — they were your neighbor, your advocate, sometimes even your dinner guest. But in 2025, that’s harder and harder to come by.
Today, centralized, corporate healthcare is accelerating. In 2024, the share of physicians working in independent practices was 42.2%, down 18% from 60.1% 2012.
Rural areas have been hit especially hard, as the total number of physicians has dropped by nearly 2,500 — and total medical practices have shrunk by about 3,300 over the last five years. During the same period, the number of independent practices in rural areas declined by 42%.

Why? Paperwork. Policy. Pressure. Small practices are being squeezed from all sides, leaving little room to actually care for patients.
At Freed, we believe small, independent practices aren’t just worth saving — they’re worth prioritizing.
Our 2025 Clinician Survey paints a clear picture: clinicians are proud of their work, ready for change, and increasingly turning to AI to help them stay independent.
What (and who) we asked
We held a survey with 1,000 U.S. clinician respondents across roles and specialties. Our goal was to better understand:
- The scale of the administrative burden
- The emotional and economic toll on small practices
- How AI is already reshaping daily work
The big picture
Clinicians enter medicine to care, not to click. And for the most part, they still love the work itself:
Clinicians love their profession
- 92% are satisfied with their career choice
- 91% feel they fulfill their purpose as caregivers
But the burden is real
- 88% spend at least 6 hours a week on admin work
- 57% spend more than 11 hours — a full day or more
- 48% hear family complaints about after-hours work
Many are reaching a breaking point
- 38% have considered cutting clinic hours
- 25% are thinking about leaving medicine entirely
And patient happiness feels at risk
- 91% believe they deliver quality care
- But only 67% think their patients feel highly satisfied
Half of clinicians have already turned to AI. Adoption is not a fringe trend. It’s a mainstream shift.
Deep dive: the reality for small practices (1–30 clinicians)
For small and independent clinics, there’s even more pressure. These clinics often run lean — without IT teams, office managers, or buffer staff to absorb the blows.
When admin demands spike, the burden lands directly on the clinician’s desk and follows them home.
Pain points
Strained by paperwork and pressure: Small-practice clinicians are acutely aware of the toll:
- 77% say paperwork is a heavy burden
- 43% say the workload is far worse than they expected when entering the field
- 49% cite declining reimbursement or policy changes as a direct threat to staying open
The human toll of carrying too much:
- 48% hear complaints from family about lost evenings and weekends
- 28% seek mental health support due to job stress
- 25% are actively weighing a complete exit from medicine

AI as a lifeline
When time is scarce and burnout is real, tools that give clinicians back even a few hours a week can be the difference between staying and stepping away.
AI isn’t some future fix — it’s already working
Nearly half (48%) of small-practice clinicians already use AI tools, and the results speak for themselves:
- 69% feel less admin burden
- 52% work fewer after-hours
- 57% report better patient care
- 51% can see more patients without staying late
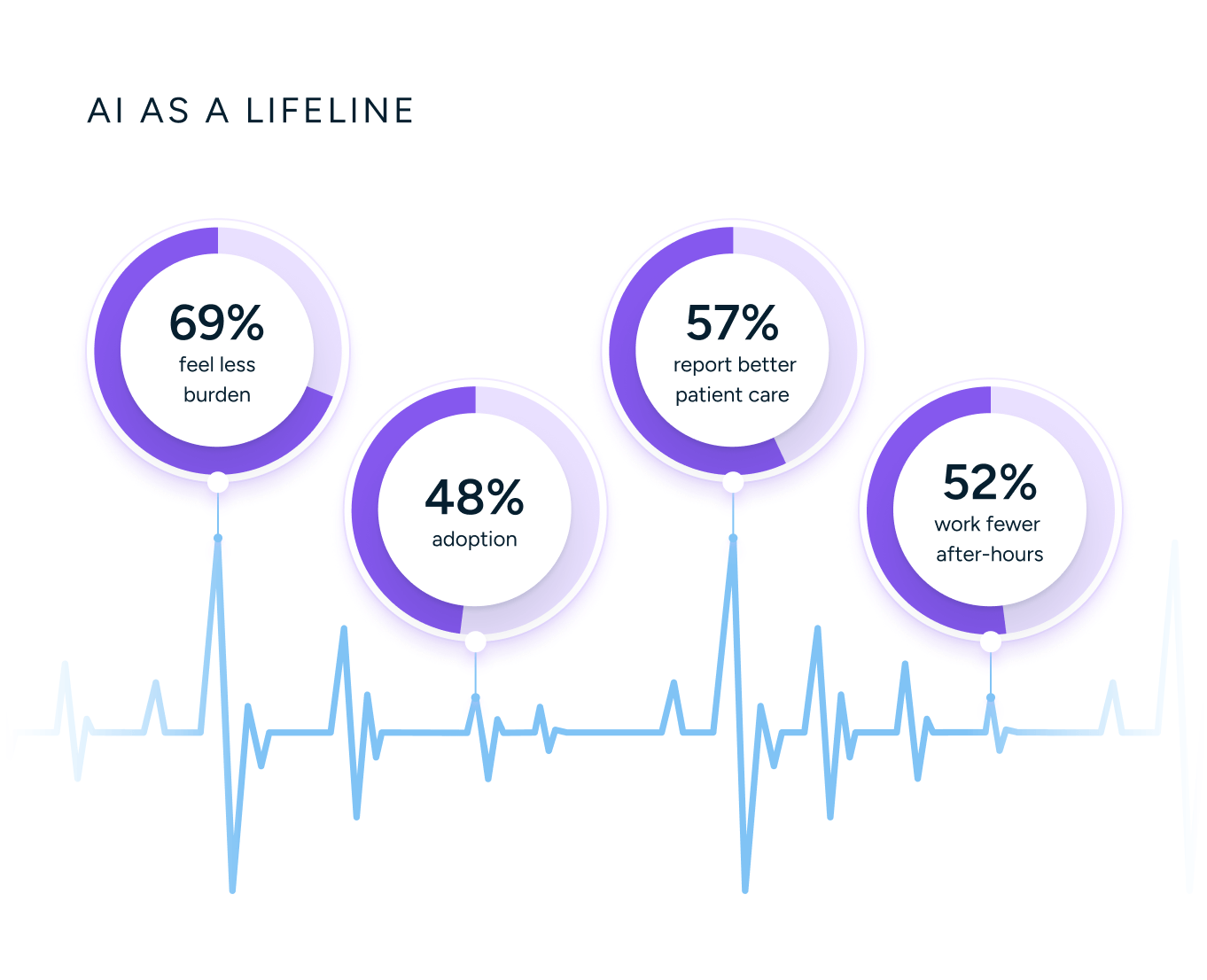
When time is scarce and burnout is real, tools that lighten the administrative and mental load can make a difference.
The whole-system view: all practice sizes
This isn’t just a small-practice problem. Burnout is spreading across the system — and so is the relief with AI.
Burnout across the board
The system is stretched thin:
- 57% of clinicians lose 44+ hours/month to documentation
- 29% are burned out or on the brink of leaving medicine
- 50% say current policy threatens their practice sustainability
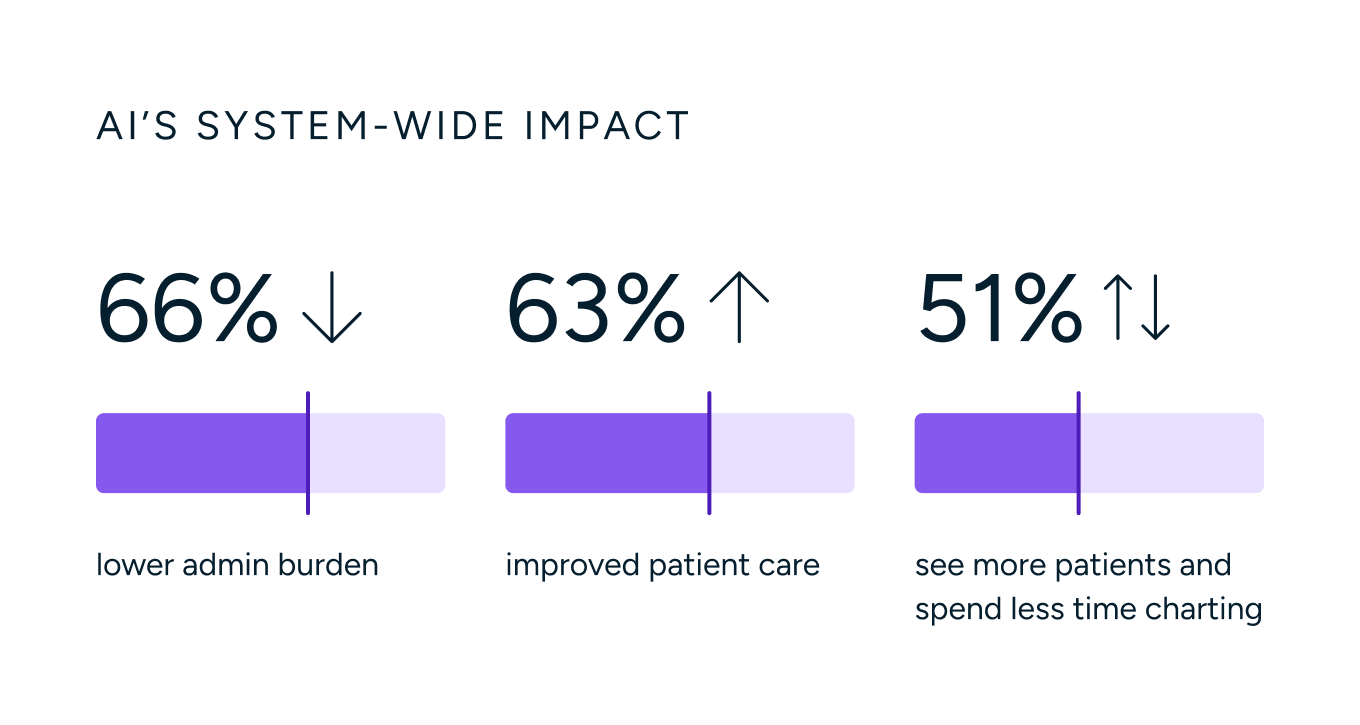
AI’s system-wide impact
And AI is already helping:
- 66% report lower admin burden
- 63% say patient care improved
- 51% see more patients and spend less time charting
Where AI fits in the day-to-day
So, what are clinicians actually using AI for? Not futuristic diagnostics or far-flung predictions. Just practical, daily help in the places it hurts most.
Among adopters, the most common use cases are:
- Appointment scheduling and reminders (49%)
- Real-time patient notes and scribing (48%)
- Inbox triage and messaging (38%)
These aren’t bells and whistles. They’re the tedious, time-sucking workflows that chip away at every hour, every visit, every evening.
That’s exactly why they matter.
Barriers still to overcome
The barrier to adoption isn’t clinician resistance. Most clinicians are ready for change. The bigger blockers? They’re mostly out of their hands.
The biggest blockers today:
- 38% — Leadership and admin sign-off
- 34% — HIPAA and privacy concerns
- 24% — Comfort in the status quo
- 20% — Patient skepticism
That’s why Freed is investing not just in product, but in partnerships and education — so small practices can adopt the tools they already want to use.
How AI is working differently across contexts
AI’s impact isn’t one-size-fits-all. It varies based on the clinician’s specialty, role, and environment. Here’s how those differences play out.
By specialty
The story shifts slightly by specialty and setting, but one thing’s clear: the more a clinician is struggling, the more AI can help.
- Most burned out: Emergency medicine: 34% burned out, lowest care satisfaction
- Most stable: Internal medicine: just 2% on the brink, highest peer recommendation rates
- Biggest gains from AI: Behavioral health: 82% feel less burdened, 76% report better care
By role/position
Physicians:
- 45% burned out or on the brink
- 69% AI adoption—highest among roles
Behavioral-health clinicians:
- 53% burned out pre-AI
- 82% feel less burdened
- 76% report better care
- 71% see more patients
By setting
Community hospitals:
- Lowest “extensive tech” rating (37%)
- Lowest AI adoption (43%)
Private practices:
- Least likely to consider leaving medicine (18%)
- Most after-hours complaints from family (52%)
- 60% reduce evening/weekend work post-AI
These early patterns point to where AI is already making a difference. But they’re just the beginning.
As more practices adopt and adapt, the use cases will grow, and so will the impact.
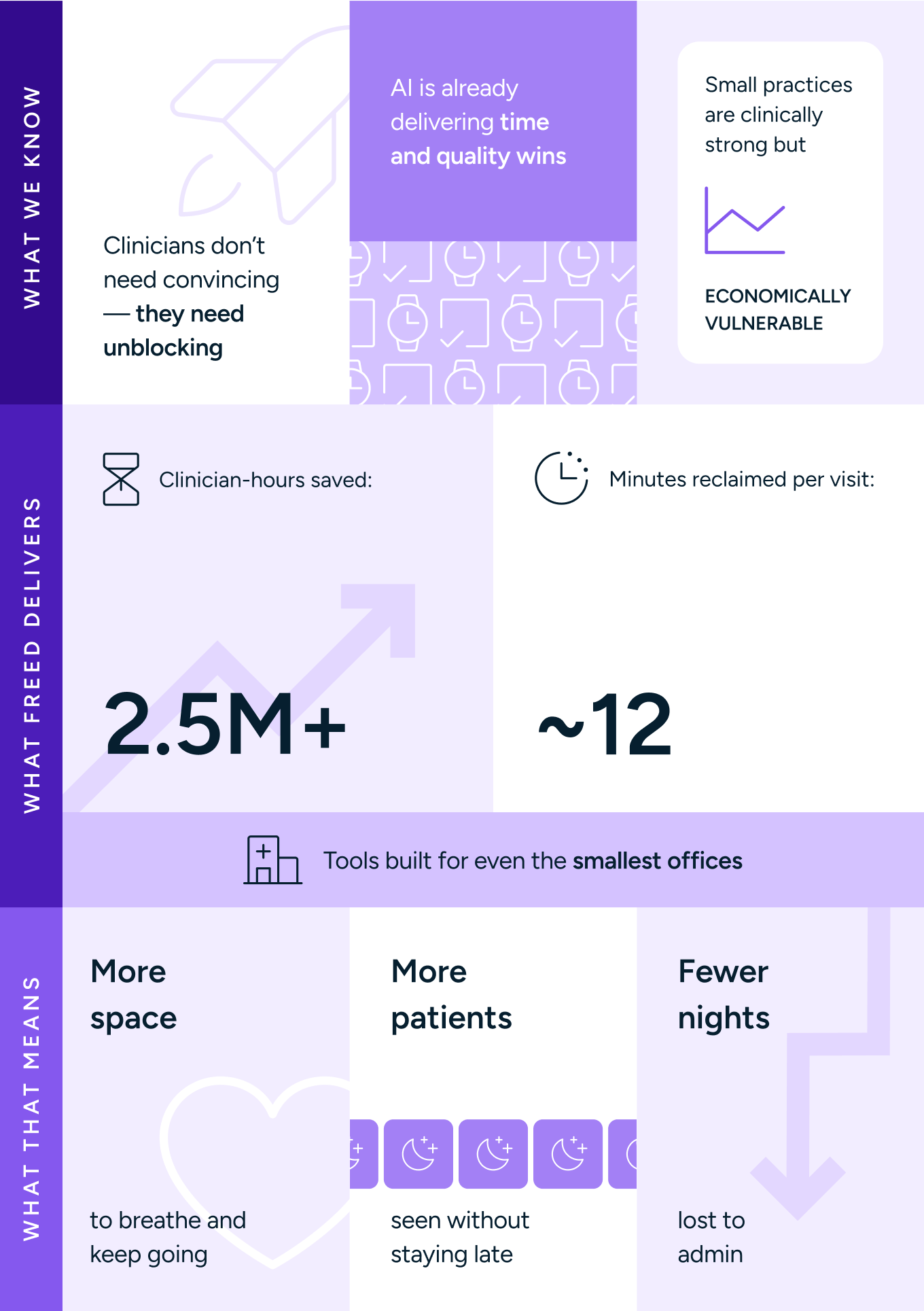
What it all points to
Small practices don't need transformation — they need room to breathe.
Here’s what we know:
- Small practices are clinically strong but economically vulnerable
- AI is already delivering time and quality wins
- We don’t need to convince clinicians — we need to unblock them
That’s why Freed exists. We weren’t built for bureaucracy. We’re here to support the clinicians actually doing the work at these small practices.
Our tools are designed for speed and simplicity for even the smallest offices. We’ve already saved over 2.5 million clinician-hours, with the average user reclaiming ~12 minutes per visit.
But the real story isn’t the numbers. It’s what happens when that time comes back: more patients seen without staying late. Fewer nights lost to admin. A little more space to keep going and find joy.
Because when we make care easier to give, we make it easier to stay.




FAQs
Frequently asked questions from clinicians and medical practitioners.





